99385 CPT Code (2023) | Description, Guidelines, Reimbursement, Modifiers & Example
99385 CPT code is a medical procedure code in “New Patient Preventive Medicine Services” and is still valid, according to the American Medical Association. During a well-patient visit, Medical care may be provided to patients between 18 and 39.
Summary Of The 99385 CPT Code
When a new patient is being evaluated and treated for preventive medicine for the first time, the CTP code can utilize. One’s medical history, examination, counseling/anticipatory guidance, and risk factor reduction efforts are all part of this evaluation and therapy. The typical fee is $120 to $150 for persons aged 18 to 39.
Regular comprehensive preventive medicine services are usually well-patient examinations for established patients who may present for reevaluations and management of their overall health, with code selection based on age.
CTP code 99385 may use for a new patient’s initial comprehensive preventative care patient background, investigation, mentoring instruction, major consideration reduction intervention strategies, and the ordering of research lab procedures.
When an anomaly or preexisting condition may discover during a preventive visit, significant applicable sections will provide at the same time as the abnormality or preexisting condition.
The Preventive Medicine service code will use on the patient medical background and provision of evaluation and management services. It will compensate for a tiny Problem-Oriented service or a code that refuses to submit with modifier 25 attached.
An individual’s plan for preventative care may or may not be included in the office visit, emphasizing that its primary purpose is to deliver treatment and not to bill separately. There can be no cost-sharing for visits to the doctors’ offices.
Description Of CPT Code 99385
Preventive medicine services focus on protecting, promoting, and preserving health and well-being and preventing infection, disabilities, and premature death for individuals and designated populations. Well-patient exams with a code selection depending on the patient’s age are often the first preventive medicine procedures for new patients who may never examine.
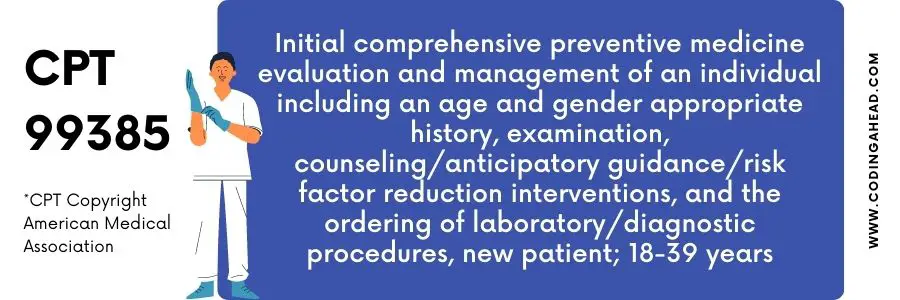
The official description of CPT 99385 is: “Initial comprehensive preventive medicine evaluation and management of an individual including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, new patient; 18-39 years.”
Any laboratory and diagnostic procedure orders are included in these services, as are the requisite patient history and examination. Preventative examination concerns or complaints that do not involve any further effort or entail performing the critical components of the problem-oriented E/M service are not required to be reported by clinicians.
There is a CTP Code 99382 that uses for children ages 1 to 4 years. It is the CTP code used for neonates under one year old. CTP code 99383 is for children ages 1 to 5 years, CTP code 99384 is for adolescents ages 12 to 17, 99385 CPT code is for adults ages 18 to 39, and CTP code 99386 is for patients ages 40 to 64.
To ensure good health, a physician conducts health screenings for Medicaid recipients ages 21 and older. Diagnose and prevent sickness, disability, and other health problems using them, and track how they’re going. Full service will include in this deal. It’s not possible to charge separately for required or recommended components.
The E/M 2021 revisions do not affect these services as they are not time-based services. Code selection for preventative service evaluations will record, as is common in such situations. As a result, time spent delivering preventive services cannot apply to time spent on problem evaluation because it cannot document twice.
The problem assessment phase of the encounter is likely to be coded using MDM. It will still be necessary to include Modifier 25 in problem assessments when providing dual E/M service before the E/M upgrades in 2021.
Billing Guidelines
Many characteristics make it difficult to generalize the immediate cost-effectiveness of preventative visits. However, comprehensive research may lead to specific practices concluding that preventive treatment benefits both the patient and the practitioner. Two CTP codes can charge together: 99385 CPT code and 99203.
Suppose a new or modified problem is addressed during a preventive service and is big enough to require extra work to do the critical parts of an issue review and strategic planning service. In that case, you must bill including both facilities with modifier 25 attached.
However, when offered as part of a distinct problem-oriented encounter, preventive medicine codes 99401-99409 may use.
Preventive treatment will be available to patients regardless of their insurance status, even if they have to pay the bill themselves. Patients aged 18 to 64 can use the “Preventative visit algorithm” to plan preventive visits (except for recommended pregnancy-related services).
These guidelines may be based on the most robust evidence-based recommendations by the United States Preventive Services Task Force. They will not design to reflect all possible preventive counsel or screenings you might give a patient.
To avoid the second service being mistakenly bundled or rejected, include a separate notice explaining it. As a reminder, no single document can not be utilized for both services simultaneously.
For example, an E/M service that demands significant time and documentation may absorb so many components of the preventive service that you don’t have a complete history and exam. Some doctors prescribe two visits in certain situations because of this exact reason.
Bundling is more common if the separate service can be considered age-appropriate, such as at the beginning of acne treatment. Preventative services will not package if an E/M note can create for the condition, according to CPT’s statement of modifier 25 and the exclusions stated for the preventive visit CPT codes.
While being remedied as part of a preventative visit, in some instances, issues requiring further work will bill separately using modifier 25; please see “Appropriate use of modifier 25 during a preventive visit” for more information.
Well-patient exams for established patients presenting for disclosure and managing their general health condition are frequently comprehensive preventive medicine services, with code selection based on age.
Reimbursement
As stated by the American Medical Association, cost-sharing for an office visit may permit if both the office visit and the eligible preventive service are separately billed, and the primary goal of both is to provide a service that may not cover by the insurance policy
Billing Examples
The following are examples of when the 99385 CPT code can be reported.
Example 1
“A 45-year-old man treated for high blood pressure at a clinic receives a cholesterol screening test as a preventative measure. There may be cost-sharing obligations for the office visit because recommended preventive care will separately bill, and the visit was not primarily for preventive services.”
Example 2
“A person obtains a recommended preventative service but is not separately charged.” A persistent stomach ache was the primary cause of the visit, not a recommended preventive procedure. As a result, the plan or issuer may ask for cost-sharing to visit the doctor’s office.”


