99395 CPT Code (2023) | Description, Guidelines, Reimbursement, Modifiers & Examples
99395 CPT Code billing is made simple with our guidelines. Preventive medicine programs are accessible to those who do not require emergency medical assistance and have a regular medical assessment as a prudent precaution.
Preventive medicine reevaluation and management services include well-baby consultations, well-woman consultations, and traditional, thorough physical examinations.
These appointments are distinctive from those in which the patient seeks immediate treatment for a condition. When offering primary care therapy, one should consider the person’s age, race, and risk factors.
The specialist thoroughly examines systems, a detailed previous family and social history, and a complete evaluation of age and gender-related determinants.
The physician may prescribe and acquire diagnostic or laboratory investigations during the study and provide vaccines.
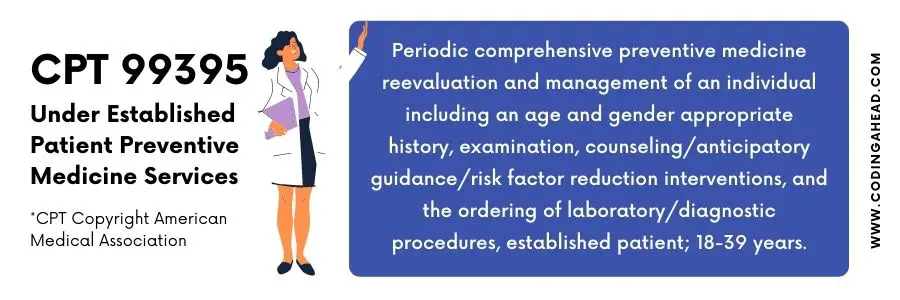
99395 CPT Code | Description
99395 CPT code is used for periodic extensive primary care reassessment and monitoring of an individual, albeit with age and gender-relevant history, evaluation, mentoring counselling element mitigation treatments. 99395 CPT code is also used for organizing clinical lab procedures established patient; delayed childhood (age 18 through 39 years).
The coder can report preventive medicine procedures for an established individual with the help of these codes. When choosing this E/M treatment, duration is not a consideration.
The individual’s age or whether the individual is new or established are used to identify which code to use.
One can distinguish E/M service if the evidence authorizes the provision of a significant, independently recognized, accurate assessment and administration service.
To specify that a physician has performed a specific and separate E/M treatment on the day of service as the preventive medicine service, add modifier 25 to the chosen service code.
Vaccinations and support facilities required at the preventative treatment, such as testing, radiography, or diagnostic tests, may be differentiated. Medicare does not fund preventive medical services.
For the provision of preventative services to a new patient.
Suppose a patient comes for admission for a regular preventive assessment. But he also has substantial additional issues (e.g., chest discomfort or irregular bleeding).
And in some instances, he has a new and existing chronic disease (e.g., hypertension or type-II diabetes).
Then, in that case, the consultation may become a mix of preventative treatment and challenge treatment.
CPT manual suggests submitting a preventive care services code for the routine exam. And the standard office consult code with modifier 25.
The modifier 25 narrates as substantial, separate, and distinct [E/M] service executed by the very same practitioner or by the other healthcare professional on the same day.
In these circumstances, it’s also critical to link the relevant ICD 10 CM to the appropriate CPT code to differentiate between preventative and problem-oriented treatments.
A thorough evaluation and assessment and age-equant anticipatory coaching are the components of preventive medicine therapy.
An extensive inspection is not the comprehensive inspection described by the 1995 or 1997 Evaluation and Management Documentation Guidelines in preventative health treatments 99381 – 99397 (including 99395 CPT code).
Furthermore, the basis for evaluation must accurately estimate the person’s age and gender.
For instance, the examination will differ for a 4 – year – old boy and a 22 – year – older woman.
For a growing kid, one must assess physiology (height, size, and head circumference) and cognitive functioning like talking, walking, and resting patterns.
Use of child seats and specific other health hazards and the introduction of new foods are examples of anticipated guidelines.
Scoliosis diagnosis, developmental assessments, and vaccine reviews are examples of youth preventative services.
Anticipatory advice might include building excellent health attitudes and self-care, discussions about substance, alcoholism, cigarette use, and sexual activities.
A gynecologic checkup, pap smear test, and chest evaluation are part of a full preventative consultation for a grownup female patient.
For elderly patients, a grownup male’s inspection might involve examinations of the scrotum, gonads, penile, and prostate.
Anticipatory counselling should identify areas like alcohol and cigarette usage, safe sex practices, diet, and activity to assist people to enhance their grades in life.
Addressing the patient’s job situation and other emotional distress is possible. Cholesterol, blood sugar, and prostate-specific antigen (PSA) tests may become more critical as patients get older.
99395 CPT Code Billing Guidelines & Reimbursement Policies
Following are the procedural codes for new patients who are visiting for a well-baby or well-child care:
Employ CPT code 99381 for infants who are under one year old.
Employ CPT code 99382 for children in the early childhood phase, i.e., from 1 to 4 years old.
Employ CPT code 99383 for children in the late childhood phase, i.e., from 5 to 11 years old.
Employ CPT code 99384 for children in their adolescent stage, i.e., 12 to 17 years old.
Employ CPT code 99385 for ages 18 to 39 years old.
Following are the procedural codes for established patients who are visiting for a well-baby or well-child care:
Employ CPT code 99391 for infants (under one year old).
Employ CPT code 99392 for children in the early childhood phase (1 to 4 years old).
Employ CPT code 99393 for children in the late childhood phase (5 to 11 years old).
Employ CPT code 99394 for children in the adolescent stage (12 to 17 years old).
Employ 99395 CPT code for ages 18 to 39 years old.
The age at diagnosis, either new or established, determines the code classification. CPT uses a three-year guideline to ascertain if a person is new or established.
We may consider the individual an established patient if any practitioner in a group practice has visited him.
More accurately, an “established” patient is; if any practitioner of the same discipline billing together under the set of numbers has seen him for an immediate treatment within the previous 36 months.
The evaluations should verify the visit’s preventive nature. Each invoiced treatment should accompany an ICD 10 code describing the program’s purpose.
You must submit so-called Z codes because there is no patient concern during a good checkup.
Medicare sometimes doesn’t pay for CPT’s broad preventive medicine therapy codes.
However, it does pay for several cancer screenings performed without sickness, condition, sign, or discomforts, such as a diagnostic genital and physical inspection, thanks to the Balanced Budget Act of 1997.
The coder must submit truthful claims. These reimbursement criteria guarantee that your claims for the health care services are according to the codes that truly describe those services.
The coder can utilize the rules and regulations provided by current procedural terminology (CPT), Centers for Medicare and Medicaid Services (CMS), or other coding rules in United Healthcare prepayments.
Contributions to CPT or other materials are solely for explanation and do not indicate entitlement to payment.
This reimbursement policy covers all medical services invoiced on CMS 1500 forms, and those invoiced on UB04 states were displayed.
In designing reimbursement criteria, one can consider coding technique, industry-standard reimbursement rationale, compliance standards, compensation structure, and other related aspects.
This material helps support a global reference guide for a compensation program for the benefits rendered. It does not purport to cover every facet of a reimbursement scenario.
As a result, it may review and understand this rule to medical services given in a specific situation with reasonable discretion.
Furthermore, the insurance does not cover all aspects of compensation in the health care system.
Other reimbursement-related considerations may augment, amend, or override this strategy in some situations.
Administrative process, professional or different practitioner agreement, the enrollee’s advent coverage papers, and reimbursement, clinical, or medication regulations are examples of these considerations.
Ultimately, one cannot administer this rule precisely with the same approach on United Healthcare’s modern digital claims processing applications due to technological and perhaps other restrictions.
Nevertheless, United Healthcare seeks to minimize these discrepancies. Every insurance company has the right to change this compensation policy occasionally by releasing a new edition.
Preventative Health Solutions have a broad scope. It incorporates age and gender adequate records and assessment.
And it also includes counseling, proactive advice, and potential risk minimization, often distinct from illness findings.
Periodically, during the preventative consultation, an anomaly or previous condition is discovered, and essential aspects of relevant Evaluation and Management (E/M) services are delivered simultaneously.
And this happens whenever the concern E/M service code is added with modifier 25; it will compensate the Preventive Medicine Cost estimation 50% of the conflict E/M service code.
The insurance can cancel the claim if the problem-oriented service is insufficient or the coder has not attached modifier 25 with the CPT code.
The insurances may only pay such a Primary Care Session when the provider delivers Preventive Medicine services and other E/M services over the same visit.
Healthcare resources include cervical cancer monitoring, hip and chest examinations, prostatic cancer screening or digital genital tests, and acquiring, developing, and transporting a prenatal screening smear to the research lab.
The Preventive Medicine Service covers these monitoring treatments provided on the same day (and are not paid separately).
How To Apply Modifiers
According to CPT, one should gather thorough information as a preventative treatment, not focus on the main issue or current disease.
Conversely, it necessitates a “complete system evaluation and continuous or intermediate personal, familial, and societal history record, and even a detailed analysis of applicable risk variables,” and therefore a “complete assessment and pertinent adverse outcomes.”
Preventative auditing and monitoring features are associated with age and health conditions instead of a considering state, instead of a problem-oriented scheduled visit.
When just under a detailed record and assessment are provided throughout a preventative treatment, a few have sought to utilize modifier 52 to signal decreased services.
Modifier 52 is solely applicable to technical services; hence, this is unsuitable.
The coder must code as E/M office visits for preventive checkups which do not meet the minimum standards.
Modifier 25 in coding may permit you to compensate with both a preventative visit and a genuine concerned E/M service or routine service provided on the same day.
According to CPT, the coder can use modifier 25 when the same physician executes a central, individually identifiable assessment and control service on the same day.
The coder must use modifier 25 if the second show involves substantial additional labor to be considered an office appointment.
The problem-oriented E/M code must usually have modifier 25 linked to it.
Append modifier with precautionary visit code since it is the E/M treatment if the second show is a procedure, including excision of a skin lesion conducted in combination with a preventative visit.
Example
The need for an ICD 10 CM code for abnormal results (e.g., Z00.121) does not need or allow the utilization of extra E/M activity.
Abnormal results might be minor or unrelated concerns that would not necessitate further investigation.
Yet, the illness is nevertheless recorded or labeled as contributing.
Atypical discoveries might include aberrant screening results, a novel acute illness, or an unsettled or deteriorating degenerative illness.
An unsatisfactory results code would not be appropriate for a stabilized chronic disease (whether handled or not). If the testing is acceptable, you can connect a major complications ICD 10 CM code to it; the aberration will be detected with the relevant ICD 10 CM code, alerting the payer.


