(2023) CPT Code 80050 | Description, Guidelines, Reimbursement, Modifiers & Examples
CPT code 80050 is a medical procedure code for organ or disease-oriented Ppanels. The lab analyst tests the general health panel’s specialized collection of clinical laboratory tests. The doctor must order the individual tests for diagnostic purposes, which is not the case if the board may perform a screening.
Summary
If the test does not impact ESRD management, the provider will provide the qualifier “AY.”As a result, these codes most accurately depict laboratory services delivered to ESRD PPS beneficiaries. Only the organs and disorders panels (80048, CPT code 80050, 80053, and 800-76) fulfill the 50% criteria.
Clinical diagnostic laboratories, on the other hand, must bill these services individually rather than in panels. Patients with CAPD end-stage renal disease (ESRD) who dialyze at home will charge the same as any other home patient for tests that may not cover by the composite rate.
Panel codes containing constituent tests from a single patient collection do not submit more than once. If a set of tests spans more than one panel, report the panel with the most tests that satisfy the code description, then write the other tests using their respective test codes (for example, don’t report 80047 alongside CPT code 80050).
Under UnitedHealthcare’s laboratory bundling policy, laboratories will no longer accept CPT 80048, the basic metabolic panel, as justification for bundling with CPT code 80050, the hepatic function panel. Mostly CTP code 80050 will use for laboratory tests and examinations, and it may combine with other codes during the billing process.
It has happened as a result of new information from CPT. It may also be consistent with CPT coding requirements. Except for CPT panel number 82248, CPT panel code 80053 has all of the features of CPT panel code 80048 and all of the elements of CPT panel code 80076. If the 80050 CPT code and CPT 82248 will use at the same time on the same day of service, they should be invoiced separately.
The advent of organ- or disease-specific lab panels made codes for various tests available. Providers must bill the lab panel when all examinations specified in each forum may perform on the same service date.
If more than one test in the forum may not serve on the same day of service, the provider may charge individually for each test. The number of tests a provider can bill for on the same day is limited. Other tests done on the same day of service, in addition to the panel code, may be reported.
Providers must use CPT coding regulations when writing on multiple panels. Because all the lab tests in basic panel code 80048 are components of comprehensive panel CPT code 80050, providers cannot record both basic panel code 80048 and complete panel code 80053 on the same service date.
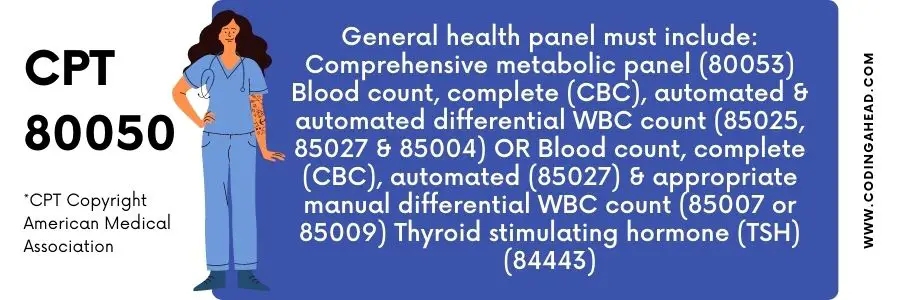
Description Of CPT Code 80050
The official description of CPT 80050 is: “General health panel.
This panel must include the following: Comprehensive metabolic panel (80053)Blood count, complete (CBC), automated and automated differential WBC count (85025 or 85027 and 85004)ORBlood count, complete (CBC), automated (85027) and appropriate manual differential WBC count (85007 or 85009)Thyroid stimulating hormone (TSH) (84443).”
If a claim includes a complete lab panel code and a more accurate code for the service provided, the computer will merge the component lab codes into the more comprehensive panel code. When the panel code is missing from the claim, multiple claim lines will disregard it in favor of a single, more comprehensive panel code.
It is not permissible to use the 80053 Comprehensive Metabolic Panel. The automatic differential WBC count, total CBC, and 85025 exclude 85025.
According to CPT coding guidelines, the 80050 CPT code General Health Panel permits you to call the CPT code 80050 General Health Code 80047 for a basic metabolic panel (calcium, ionized) should not be coupled with CPT code 80053.
Even though the original application already included CPT 80047, the services must be re-submitted with CPT 80053 may reimburse.
CPT code may use in conjunction with CPT code 80053. When CPT 80048 and CPT 80053 are submitted simultaneously, only CPT 80053 will reimburse. There are two alternatives for the CPT code 80048 for a Basic Metabolic Panel (total calcium):
Panel codes are integrated into one comprehensive panel code when a claim is submitted with the service done and a correct panel code. Having a single panel code for all claims is preferable to having numerous lines for each share. As a result, using the 80053 Comprehensive Metabolic Panel is unsuccessful.
- The total CBC, 85025, or automated differential WBC count, does not include 85025.
- Restriction on the Use of Thyroid-Stimulating Hormones
Billing Guidelines
The CPT code 80047 for the Basic Metabolic Panel offers many options. The CPT code 80050 General Health Panel can use for a basic metabolic panel (calcium, ionized), but 80047 and 80053 will not. Although CPT 80047 include in the first application, CPT 80053 may consist of getting paid for the services.
Suppose the same doctor or another healthcare practitioner also submits CPT code 82330 and at least four of the following laboratory codes on the same day of treatment. CPT code 80050 Basic Metabolic Panel (Calcium, Ionized) payment will award in that case.
According to CPT coding guidelines, CPT code 80048 will not be used with CPT code 80053. If CPT 80048 and 80050 may submit at the same time, only 80053 will pay. For the CPT code 80048 for a Basic Metabolic Panel (total calcium), there are two options:
- A Basic Metabolic Panel is an 80048 service comprising at least five laboratory component codes.
- It may conduct by the same physician or another healthcare professional on the same day for a single patient (Calcium, total).
The computer can integrate component lab codes into a complete panel code if the claim includes a correct service code and a more thorough panel code. As a result, using the 80053 Comprehensive Metabolic Panel is unsuccessful. The total payment for 85025, or automated differential WBC bill, does not include 85025.
Billing Examples
The following are two examples of when CPT code 80050 can be used. .
Example 1
A blood glucose meter test may order for a patient examined in the emergency room. The doctor requests another BGM lab test at another session to get a different accession and result code. A 80050, 82962-91 code would be appropriate for this interaction.
Example 2
An older man with diabetic ketoacidosis underwent a series of blood tests to determine whether or not potassium supplementation and low-dose insulin therapy improved his potassium levels. Three further blood tests were requested and performed on the same date as the initial potassium results to monitor his blood levels while the potassium treatment progressed.