90834 CPT Code (2023) | Description, Guidelines, Reimbursement & Modifiers
The 90834 CPT code is used to code psychotherapy services and procedures and is still current, according to the American Medical Association. Patients with mental health issues can receive psychotherapy from this service provider. The patient’s therapy session varies from 38 to 52 minutes.
Description Of The 90834 CPT Code
Therapy dynamics can reveal by 90834 CPT code documentation of treatment plan modifications. The primary goal of CPT codes for psychotherapy is to ensure that insurance companies adequately compensate for the services rendered. In other words, follow the rules if you want to pay reasonably.
The official description of CPT code 90834 is: “Psychotherapy, 45 minutes with patient.“
There are time-based codes for psychotherapy services (CPT codes 90832-90838). These codes use whenever a start or end time is and the overall amount of time spent. Medical justification for each psychotherapy session must be documented in the 90834 CPT code medical record papers.
One of the legitimate issues in physiotherapy is using E/M services in combination (CPT codes 91833-91836-90838). E/M service start and end timings and the total duration of psychotherapy will document due to the time-sensitive nature of psychotherapy. It would also be necessary to keep track of each therapy session’s start and stop times.
When a physician or NPP provides psychotherapy and E/M treatments, the paperwork should demonstrate that the two differ. Meetings with a therapist take place face-to-face with the person who will treat.
An emotional or behavioral condition or symptoms that are severe enough to alter one’s normal state of functioning and comprehensive session documentation, including instances of therapeutic interventions such as behavior change attempts, supportive participation, and discussions of reality;
Documentation of the therapist-patient relationship requires an evaluation of the patient’s problem (s). Psychotherapy billing codes 90834 and 90837 are both available. 90834 refers to 45 minutes of psychotherapy, whereas 90837 refers to 60 minutes.
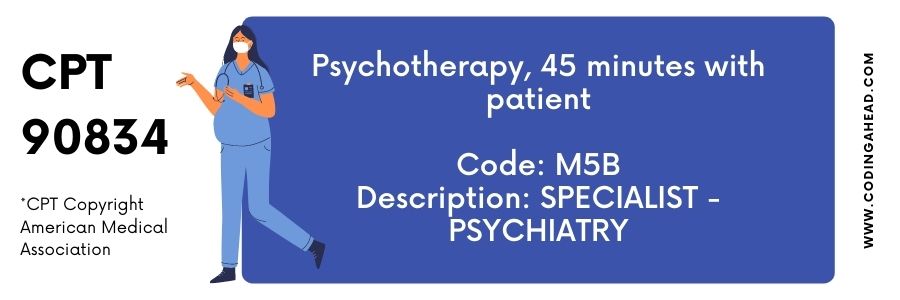
CPT code 90834 covers psychotherapy for 45 minutes. Services hold due to a lack of consistency in reporting the medical documents submitted. 90834 CPT code is a telemedicine code in the merit-based incentive payment system.
Measurable goals will include in the treatment plan. The patient’s ability to participate in and benefit from psychotherapy is documented regularly in the documentation for the 90834 CPT code. A full report of the psychotherapy sessions is required.
Regular documentation of the estimated treatment duration should include the number of sessions needed, the target symptoms, and the measurable and objective therapy goals related to changes in behavior or thought processes and medications.
There should also be documentation of the methods of outcome monitoring and why the chosen therapy is an appropriate modality in place of another type of psychiatric treatment. These are the codes for psychotherapists without psychiatric examination and management services: 90832, 90834 CPT code, and 90837, respectively.
There have been improvements in the patient’s symptoms or behavior since the last session and progress toward measurable goals. Therapy dynamics can reveal by CPT 90834 documentation of treatment plan modifications.
Neither of these codes intends to capture any administrative aspects of therapy sessions, such as collecting copays, planning future visits, or writing notes.
Billing Guidelines
Neither of these codes intends to capture any administrative aspects of therapy sessions, such as collecting copays, planning future visits, or writing notes. The 90834 CPT code will be used for sessions lasting 38–52 minutes and 90837 for sessions lasting at least 53 minutes.
A 50-minute therapy session will charge 90834 CPT code, but you will pay 90837 for longer sessions. Staff employees who handle health billing are nearly always found in hospitals and large private practices.
The story’s lesson is to ensure that you fill out all of the information requested by the billing department. They cannot fill out codes without the proper knowledge, even though they are usually very good at doing so. If you don’t fill out all the needed codes, the staff may get angry, delaying your payment.
An emotional or behavioral condition or severe symptoms alter one’s normal functioning. Suppose the patient is actively involved and regularly communicates with their therapist. Documentation of therapy interventions such as examples of behavior modification, supportive participation, and reality talk; and a thorough account of the session
The medical record should detail any variation from the treatment plan or treatment prolongation. In addition to assessing the patient’s problem, a therapist must chronicle the patient-therapist connection (s). For example, you can use dolls or other toys in your treatment sessions.
The following are the three most common contributing CPT cases to use when billing for the 90834 CPT code:
- In some cases, the expense of this interactive complexity add-on code may not be deductible. This rating denotes the difficulty of the treatment.
- Outside of regular business hours or on days when the office is usually closed, services provides at the office.
Using Modifiers With The 90834 CPT Code
The service provides the new CPT modifier for “synchronous telemedicine” using a real-time interactive audio and visual telecommunications infrastructure. Modifier 95 is added to the primary code to indicate that the patient receives behavioral health teletherapy.
For example, if you add 95 to CPT code 90834, you’ll get a 45-minute teletherapy session (i.e., 90834-95). You must have a face-to-face video conference for this modification to appear on your invoice.
Modifier 95 indicates synchronous telecommunication services provided to the patient when billing private payers. However, texting is still not billed as a service in the United States. You must have your clients sign a telehealth consent form before providing teletherapy services.
Use the CPT code 90834 with modifier 95 when 45 minutes of psychotherapy delivers via telemedicine with the originating place of service code (typically “11” for the practitioner’s office) included
Modifier 95 will not accept by Medicare or Medicaid. Unlike the GT modifier, the Modifier 95 recognizes by all pay-out providers. In selecting a modification for your claim, the rules engine can aid.
The critical information will convey during a face-to-face interaction between a physician or other qualified healthcare professional and the patient for the significant components and needs of the same service to meet when delivered via synchronous telemedicine.
Family psychotherapy methods will record on form 90846 (without the patient present) or 90847 (with the patient present) (with the patient present). 90832 and 90833 can be reported on the same day as codes 90846 and 90847 if the services are separate and distinct. To emphasize that the services are different, use modifier 59.
When an E/M service pays with a psychotherapy session, the service’s length requires records (i.e., add-on CPT codes 90833, 90836, and 90838). If the psychotherapy treatment isn’t provided alongside an E/M service but is at least 90 minutes long and contains direct patient contact, a doctor or other qualified health care professional can submit an extended service code for CPT code 90837 (psychotherapy, 60 minutes with patients).
Reimbursement
Insurance companies keep a close eye on how you bill for services. If you’re trying to save money or make more money, don’t strive to under code or overcome (for example, billing a 60-minute session when it was just 45 minutes). You could be charged with fraud and have your insurance panel removed if you supply incorrect codes.
- 90834 CPT code – 2021 Medicare Payable at the following %: $103.28
- 90834 CPT code The Medicare 2020 reimbursement rate is $94.55 per month.
From 2020 to 2021, the reimbursement rate rose by 9.2 percent.



