(2022) How To Code Dysphagia ICD 10 – List With Codes & Guidelines
Dysphagia ICD 10 coding is made easier with our billing guidelines. This article includes all medical codes you will need to report Dysphagia and related specific ICD 10 & 11 codes, such as oropharyngeal dysphagia and dysphagia following stroke.
Read on to get a summary of the necessary codes followed by a further description.
What Is Dysphagia?
Dysphagia is a problem with swallowing that makes it difficult to get food or drink from your mouth to your stomach. Dysphagia is a painful condition. Swallowing can be difficult in several instances.
Having trouble swallowing on occasion, such as when you eat too quickly or don’t chew your food thoroughly, is usually not cause concern.
On the other hand, persistent dysphagia might be a significant medical problem that needs treatment.
Swallowing appears to be straightforward, but it is quite difficult.
This is because your brain, various nerves and muscles, two muscular valves, and an open, unconstricted esophagus (swallowing tube) are required to function properly.
Dysphagia can strike anyone at any age, but it is more common among the elderly and people with certain neurological abnormalities.
Swallowing issues have a variety of origins, and treatment varies depending on the cause.
Dysphagia can cause the following signs and symptoms:
Swallowing discomfort
swallowing difficulties
Food becomes caught in the throat, chest, or behind the breastbone (sternum)
Drooling
Hoarseness
Food is resurfacing (regurgitation)
Heartburn that occurs frequently
Backing up of food or stomach acid into the throat
Loss of weight
Swallowing causes coughing or gagging.
If you have trouble swallowing regularly or your dysphagia is accompanied by weight loss, regurgitation, or vomiting, see your doctor.
Causes
Dysphagia can be caused by any disorder that weakens or destroys the muscles and nerves involved in swallowing or that causes a constriction of the back of the throat or esophagus.
Dysphagia is classified into one of the following groups.

Oesophagal Dysphagia
After you’ve started swallowing, you may experience esophageal dysphagia, which is the sensation of food sticking or becoming lodged in the base of your throat or your chest.
The following are some of the reasons for esophageal dysphagia:
Achalasia – The conditions where food can come back up into the throat of the lower esophageal muscle (sphincter) do not relax sufficiently to allow food to reach the stomach.
Stricture of the esophagus – A stricture (narrowing of the esophagus) can capture large chunks of food. the narrowing could be from a tumor or tissue scarring from gastroesophageal reflux disease (GERD)
Scleroderma – The lower esophageal sphincter can be weakened by the formation of scar-like tissue, which causes rigidity and hardening of tissues.
Radiation therapy – is a type of treatment in which the patient is exposed. Inflammation and scarring of the esophagus may result from this cancer treatment.
Oropharyngeal Dysphagia
When you start to swallow, certain conditions might weaken your throat muscles, making it harder to transport food from your mouth into your throat and esophagus.
Causes include:
Disorders of the nervous system – Dysphagia can be caused by various conditions, including multiple sclerosis, muscular dystrophy, and Parkinson’s disease.
Zenker’s diverticulum (pharyngoesophageal diverticulum) – A tiny pouch forms in the throat that accumulates food particles, usually slightly above the esophagus. causing a problem with swallowing
Neurological damage – Includes stroke or other sudden damage to the brain and spinal cord.
Treatment includes taking a full history, physical examination, and investigation, which includes barium swallow test and endoscopy to identify the cause, and alleviation of causative factor is the mainstay of treatment.
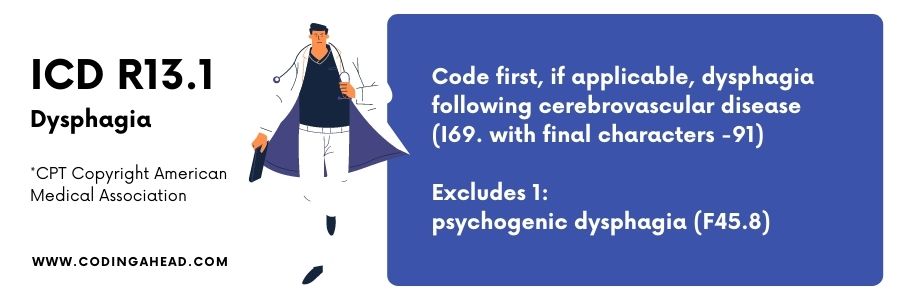
Dysphagia ICD 10
Dysphagia ICD 10 is coded as R13- aphagia, and dysphagia is a billable/specific ICD 10 CM code that can be used to indicate a diagnosis for reimbursement purposes.
It is located in chapter XVIII Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified R00-R99, under block Symptoms and signs involving the digestive system and abdomen R10-R19.
Includes:
Aphasia R13.0
Dysphagia unspecified R13.10
Dysphagia, oral phase R13.11
Dysphagia oropharyngeal phase R13.12
Dysphagia, pharyngeal phase R13.13
Dysphagia, pharyngoesophageal R13.14
Other dysphagia R13.9
Oropharyngeal Dysphagia ICD 10
Oropharyngeal dysphagia ICD 10 is coded as R13.12 of subcategory dysphagia, oropharyngeal phase. It is a billable code.
On October 1, 2021, the 2022 edition of ICD-10-CM R13.12 went into effect.
This is the ICD-10-CM version of R13.12 for the United States; other international versions of R13.12 may differ.
Esophageal Dysphagia ICD 10
Esophageal dysphagia ICD 10 is coded as R13.14 of subcategory dysphagia, pharyngoesophageal. Therefore, it is a billable code.
ICD 10 Code For Dysphagia Due To CVA
ICD 10 code for dysphagia due to CVA is I69.391 dysphagia following cerebral infarct, which Is a billable code,
located in chapter IX Diseases of the circulatory system I00-I99, under block Cerebrovascular disease I60-I69, category Sequelae of cerebrovascular disease I69-.
Synonyms include:
Previous stroke-causing dysphagia (difficulty swallowing).
Dysphagia as a late complication of cerebrovascular accident.
Oral Dysphagia ICD 10
Oral dysphagia ICD 10 is coded as R13.11 dysphagia, oral phase.
Pharyngeal Dysphagia ICD 10
Pharyngeal dysphagia ICD 10 is coded as R13.13 dysphagia pharyngeal phase.
Dysphagia With Aspiration ICD 10
Dysphagia with Aspiration is coded as R13.10 dysphagia, unspecified, which is the primary diagnosis, and aspiration being the complication, is coded as T17.400.
Aspiration is one of the complications of dysphagia. When anything unintentionally enters your airway or lungs, this is known as aspiration.
It could be food, liquid, or something else. This can result in major health issues, including pneumonia.
Unspecified foreign body in trachea causing asphyxiation .located in chapter XIX injury poisoning and other external consequences of external causes S00-T88,
block foreign body’s foreign body entering through natural orifices T15-T19, category foreign body in respiratory tract T17.
ICD 10 Code For Dysphagia Unspecified
ICD 10 code for dysphagia unspecified is coded R13.10.
Synonyms include:
Dysphagia (difficulty swallowing)
Impaired swallowing
Odynophagia (painful swallowing)
Swallowing painful
Swallowing problem
Dysphagia Due To Radiation ICD 10
Oncologic treatments for head and neck cancer, such as curative radiotherapy and chemoradiation, can result in long-term swallowing difficulties (dysphagia), which can significantly influence the quality of life.
Radiation-induced dysphagia is characterized by a wide range of anatomical, mechanical, and neurological abnormalities, polyneuropathy could have autonomic manifestation such as difficulty in eating and swallowing.
It is a neurological abnormality associated with long term radiation. It is coded as G62.82 radiation-induced polyneuropathy, located in chapter VI disease of the nervous system G00-G99,
under the blockpolyneuropathiess and other disorders of the peripheral nervous system G60-G65, category other and unspecified polyneuropathies G62.
Synonyms include radiation polyneuropathy.
ICD 10 Neurogenic Dysphagia
ICD 10 neurogenic dysphagia is coded as R13.19 other dysphagia.
Therefore, a billable/specific ICD-10-CM code can indicate a diagnosis for reimbursement purposes.
Synonyms include cervical dysphagia and neurogenic dysphagia.
R13.19 excludes psychogenic dysphagia.

Dysphagia Following A Traumatic Brain Injury ICD 10
Following a severe traumatic brain injury, dysphagia, or difficulty swallowing, is a common condition linked to an increased risk of malnutrition and pneumonia.
Cognitive and communication problems complicate the management of patients with dysphagia after a head injury.
Traumatic brain injury (TBI) and its sequelae are major causes of death and morbidity around the world.
Located in chapter XIX injury poisoning and certain other consequences of external causes S00-T88, block injuries to the head S00-S09, category intracranial injury S06 Psychogenic dysphagia.
Psychogenic dysphagia is a rare and poorly understood swallowing disorder with no anatomical or organic basis.
The dread of swallowing appears to be the most common symptom.
Malnutrition and weight loss can come from refusing to swallow certain foods, fluids, or medicines.
Psychogenic dysphagia is coded as F45.8 Other somatoform disorders.
It is a billable code located in chapter V mental, behavioral, and neurodevelopmental disorders F01-F99, under block anxiety dissociative,stress-related,
somatoform and non-psychotic mental disorders F40-F48, category somatoform disorders F45-.
Synonyms include:
Psychogenic dysmenorrhea
Psychogenic dysphagia, including ‘globushysterics.’
Psychogenic pruritus
Psychogenic torticollis
Somatoform autonomic dysfunction
Teeth grinding
Dysphagia ICD 11
Dysphagia ICD 11 is coded as ICD MD93, located in chapter 21 symptoms, signs, or clinical findings, not elsewhere classified.
Block:
Symptoms signs or clinical findings of the digestive system or abdomen (blockL1-MD8).
Symptoms or signs involving the digestive system or abdomen (blockL2-MD8).
Symptoms related to the upper gastrointestinal tract (blockL3-MD9).
Inclusive :
Incl. related to MD93
- Difficulty in swallowing
Exclusives:
excl related to MD93
Functional swallowing disorder (DD90.1)synonyms
Cervical dysphagia
Deglutions muscle paralysis
Difficulty in swallowing
Difficulty in swallowing NOS
Dysphagia, oral phase
Dysphagia, oropharyngeal phase
Dysphagia, pharyngeal phase
Dysphagia, pharyngoesophageal phase
Neurogenic dysphagia
Dysphagia Disorders (TM1)
It is coded as ICD SA50, located in chapter 26 supplementary chapter traditional medical conditions-module I Block:
Traditional medicine disorders (TM1) (BlockL1-SAO)
Organ system disorders (TM1) (BlockL2-SAO)
Spleen system disorder (TM1) (BlockL3-SA5)
Inclusive:
Incl .related to SA50
Choke disorders (TM1)
Synonyms:
- Choke disorder
- Dysphagia disorder
Functional Swallowing Disorders
It is coded as ICD DD90.1, located in chapter 13, digestive system disease, under block functional gastrointestinal disorders (block-DD9).
Inclusives:
Incl related to DD90:
- Functional dysphagia
Exclusives:
Exclusives related to DD90:
Bodily distress disorders (6C20)
Hypochondriasis (6B23)
Excl. related DD90.1
- Dysphagia NOS (MD93)
Synonyms :
Failure of swallowing function
Functional dysphagia
Functional Swallowing disorder
– Dr. Quazim Omisore,
Medical Professional & Coding Expert


