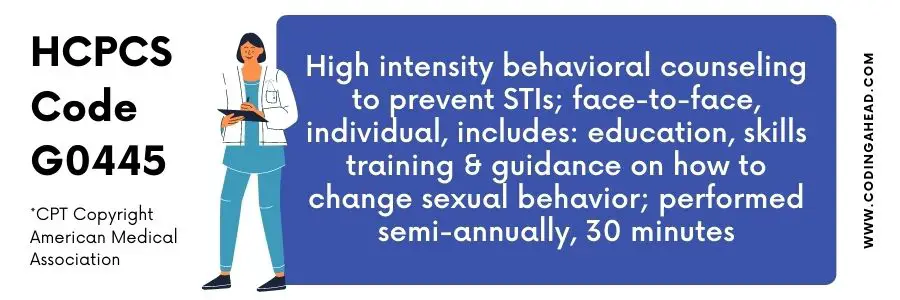
HCPCS Code G0445 Description, Guidelines, Reimbursement, Modifiers & Examples
HCPCS code G0445 bills for service when the Physician provides counseling for Semiannual high-intensity behavior to prevent STIs, Individual, face-to-face, including the guidance, education, skill training on how to alter sexual behavior.
HCPCS Code G0445 Summary
The following are the reasons why HCPCS code G0445 considers reimbursable by The United States Preventive Services Task Force (USPSTF):
– Patients at high or increased risk of sexual activity
– Had sex with multiple partners
– Careless about protection measures
– Having sex for the sake of drugs
– Had sex for extra money or drug, the age limit is 24 or below for sexually active women to screen for gonorrhea and chlamydia.
The Individual Had an STI prior and IV drug use (hepatitis B only).
The health care provider always determines the factors influencing the individual sex behavior, if any individual is more likely at risk of sexually transmitted disease.
The following Five A’s approach plays a significant role in Behavioral counseling interventions by USPSTF:
Assess: Retrieve information from the patient regarding behavioral health risk(s), factors that influence the behavioral change, goals, and methods.
Advice: Provide suggestions to alter specific and personalized behavior and information regarding health harms and benefits.
Agree: Jointly, choose reasonable treatment goals and methods that engage the patient and willingness to alter the behavior.
Assist: Utilize different behavior change methods and techniques, and support the patient to achieve goals by acquiring confidence, skills, and social/environmental. Additional treatment can apply if required.
Arrange Schedule follow-up sessions in person or by telephone) to monitor the behavior, plan the treatment accordingly, and aid ongoing assistance/support. ICD 10 code supports the medical necessity of service. Physicians can refer patients for unique or more complex treatment.
Description
HCPCS code G0445 bills for service when the Physician provides counseling for Semiannual high-intensity behavior to prevent STIs, Individual, face-to-face, including the guidance, education, skill training on how to alter sexual behavior.
Reimbursement
A maximum of one unit of HCPCS code G0445 can be billed on the same date of service, while two bills when documentation supports the medical necessity of HCPCS G0445.
The cost and RUVS of HCPCS G0445 will be $24.69 and 0.71338, respectively, when performed in the facility. In comparison, non-facility will be $29.97 and 0.86613, respectively.
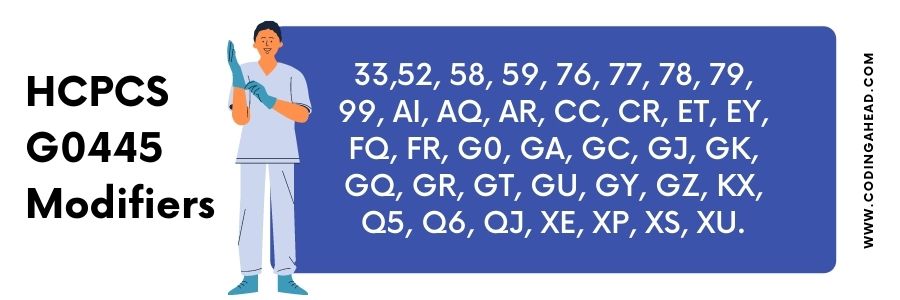
Modifiers
Modifier 52 applies when the Physician does not complete the session. The service terminates due to unavoidable circumstances.
Modifier 33 attaches to G0445 if the reason for the encounter is preventive or screening purpose only and service necessarily the requirement US government. It is applicable for commercial insurance only.
Modifier 76 applies to the HCPCS code G0445 when a similar service performs by the Same Physician on the same day. In contrast, modifier 77 is appropriate when a procedure repeats on the same date service by a different physician.
Modifier 78 will be appended with HCPCS code G0445 if the procedure repeats for an identical condition in the global period. For instance, the patient had surgery for cornea tissue removal and saw by a physician for surgery-related issues.
In contrast, modifier 79 is applicable when the service reports for an unrelated condition, e.g., a Patient seen by the Physician in the post-operative period for a headache instead of Cornea surgery-related issues.
Modifier 59 is applicable with HCPCS code G0445 if any other procedure performs in combination with these services. They do not typically play together on the same date of service. Moreover, modifier 59 will be appropriate, or service performs on the different service on the same day.
Billing Guidelines
Documentation should support the medical necessity of service or be medically appropriate. It reflects that counseling service is medically necessary and appropriate. The most used ICD codes are as follows:
- Z70.0, Z70.1, Z70.2, Z70.3, Z70.8, Z70.9, Z72.51, Z72.52, and Z72.53.
CMS allows screening of non-pregnant sexually active women who is 24 year or older women and at elevated risk for chlamydial infection
CMS allows screening of pregnant woman who is 24 year or older women and at elevated risk for chlamydial infection
CMS allows screening of all sexually active women. Additionally, Pregnant women are at elevated risk for gonorrhea infection.
CMS allows screening of pregnant women. Moreover, all individuals are at elevated risk for syphilis infection.
CMS allows screening of pregnant women for hepatitis B virus (HBV) infection at the first prenatal visit.
CMS allows HIBC screening to prevent STIs for all sexually active adolescents and those at increased risk.
Examples
The following are the examples when HCPCS code G0445 bills:
Example 1
A 17-year-old male presents to the office for sexually transmitted infection screening. He had sex with multiple partners in the past months. He was not strictly following the preventive measures.
The patient denies any recent travel, dizziness, nausea, vomiting, extremity swelling, headache, numbness, chest pain, shortness of breath, and urinary problem.
The physical exam was unremarkable. The Physician asks him about his personal life and retrieves his past and social family history. The Physician guides him to use preventive measures and avoid sex with multiple partners strictly.
The Physician scheduled a follow-up visit on the phone to monitor his behavior and take corrective action in the future. He convinces the patient to do the preventive measure in the future and get in contact with him.
Example 2
A 30-year-old female presents to the office for chlamydial infection screening. He had sex with multiple partners in the past months for the sake of drugs and got IV drugs.
He was not strictly following the preventive measures. She suspects that she is more prone to sexually transmitted infections.
The patient denies any recent travel, dizziness, nausea, vomiting, extremity swelling, headache, numbness, chest pain, shortness of breath, and urinary problem.
The physical exam was unremarkable. The Physician asks him about his personal life and retrieves his past and social family history. The Physician guides him to use preventive measures and avoid sex with multiple partners strictly.
The Physician scheduled a follow-up visit on the phone to monitor his behavior and take corrective action in the future. He convinces the patient to do the preventive measure in the future and get in contact with him.
Example 3
A 20-year-old female presents to the office for gonorrhea infection screening. She was not strictly following the preventive measures.
He realized after two days when his boyfriend told him that he had sex with a stranger girl and, more likely, she had gonorrhea and did not use protection during sex.
The patient denies any recent travel, dizziness, nausea, vomiting, extremity swelling, headache, numbness, chest pain, shortness of breath, and urinary problem.
The physical exam was unremarkable. The Physician asks him about his personal life and retrieves his past and social family history. The Physician guides him to use preventive measures and avoid sex without protection.
The Physician scheduled a follow-up visit on the phone to monitor his behavior and take corrective action in the future. He convinces the patient to do the preventive measure in the future and get in contact with him.
Example 4
A 15-year-old female presents to the office for sexually transmitted infection screening. She was fully drunk and not aware of anything. She suspected that she had sex with an unknown person at yesterday’s party.
He cannot remember anything and suspects that he is at higher risk of an STD.
The patient denies any recent travel, dizziness, nausea, vomiting, extremity swelling, headache, numbness, chest pain, shortness of breath, and urinary problem.
The physical exam was unremarkable. The Physician asks him about his personal life and retrieves his past and social family history. The Physician guides him to use preventive measures and avoid sex with a stranger and unknown persons.
He did not remember and was careless about the protection.
The Physician scheduled a follow-up visit on the phone to monitor his behavior and take corrective action in the future. He convinces the patient to do the preventive measure in the future and get in contact with him.
Example 5
A 25-year-old male presents to the office for sexually transmitted infection screening. He was involved in taking drugs and adult activities with other men. He suspects that the other Individual had sex with him when he was unconscious.
The patient had urinary symptoms for the past few days. The patient denies any recent travel, dizziness, nausea, vomiting, extremity swelling, headache, numbness, chest pain, or shortness of breath.
The physical exam was unremarkable. The labs and pathology tests confirm that patient had STD. The Physician educates the patient on how to train himself during the treatment phase.
The Physician asks him about his personal life and retrieves his past and social family history. The Physician guides him to use preventive measures and avoid sex with multiple partners strictly.
The Physician scheduled a follow-up visit on the phone to monitor his behavior and take corrective action in the future. He convinces the patient to do the preventive measure in the future and get in contact with him.
HCPCS Code G0445 Information
Effective for dates of service on or after November 8, 2011, the Centers for Medicare & Medicaid Services (CMS) will cover screening for Sexually Transmitted Infections (STIs) – specifically chlamydia, gonorrhoea, syphilis, and hepatitis B – with the appropriate Food and Drug Administration (FDA) approved/cleared laboratory tests when ordered by the primary care provider.
The tests must be used consistent with FDA approved labelling and in compliance with the Clinical Laboratory Improvement Act (CLIA) regulations and performed by an eligible Medicare provider for these services.
In addition, Medicare will cover High Intensity Behavioral Counseling (HIBC) to prevent STIs. Ensure that your billing staffs are aware of these changes.
A new Healthcare Common Procedure Coding System (HCPCS) code, G0445 HCPCS Code Description (high-intensity behavioural counseling to prevent sexually transmitted infections, face-to-face, individual, includes: education, skills training, and guidance on how to change sexual behavior, performed semi-annually, 30 minutes), has been created for use when reporting HIBC to prevent STIs, effective November 8, 2011.
This code is included in the January 2012 Medicare Physician Fee Schedule Database (MPFSDB) and Integrated Outpatient Code Editor (IOCE) updates.
ICD 9 CM Information
The appropriate screening diagnosis code (ICD 9 CM V74.5 (screening bacterial – sexually transmitted) or V73.89 (screening, disease or disorder, viral, specified type NEC), when used with the screening lab tests identified by Change Request (CR) 7610, will indicate that the test is a screening test covered by Medicare.
Diagnosis code V69.8 (other problems related to life style) is used to indicate that the beneficiary is at high/increased risk for STIs.
Providers should also use V69.8 for sexually active adolescents when billing G0445 counseling services.
Diagnosis codes V22.0 (supervision of normal first pregnancy), V22.1 (supervision of other normal pregnancy), or V23.9 (supervision of unspecified high-risk pregnancy) are also to be used when appropriate.
Specialty Types
Effective for dates of service on or after November 8, 2011, contractors shall allow screenings for chlamydia, gonorrhoea, and syphilis when reported with ICD 9 code V74.5; and/or hepatitis B when reported with ICD 9 code V73.89, only when ordered by a primary care practitioner (physician or non-physician) with any of the following specialty codes on the provider’s enrolment record:
01 – General Practice
08 – Family Practice
11 – Internal Medicine
16 – Obstetrics/Gynaecology
37 – Paediatric Medicine
38 – Geriatric Medicine
42 – Certified Nurse Midwife
50 – Nurse Practitioner
89 – Certified Clinical Nurse Specialist
97 – Physician Assistant
Place of Service
Contractors shall pay claims for HCPCS code G0445 only when services are provided for the following place of service (POS):
11- Physician’s Office
22 – Outpatient Hospital
49 – Independent Clinic
71- State or local public health clinic
Type of Service
The type of service (TOS) for HCPCS code G0445 (G0445 HCPCS Code Description) is 1.
Coverage Limitations
This code may be paid on the same date of service as an annual wellness visit (AWV), evaluation and management (E&M) code, or during the global billing period for obstetrical care, but only one G0445 may be paid on any one date of service.
If billed on the same date of service with an E&M code, the E&M code should have a distinct diagnosis code other than the diagnosis code used to indicate high/increased risk for STIs for the HCPCS code G0445 service.
An E&M code should not be billed when the sole reason for the visit is HIBC to prevent STIs.
Contractors shall deny claims for HCPCS code G0445 that are submitted without V69.8.
The use of the correct diagnosis code(s) on the claims is imperative to identify these services as preventive services and to show that the services were provided within the guidelines for coverage as preventive services.
The patient’s medical record must clearly support the diagnosis of high/increased risk for STIs and clearly reflect the components of the HIBC service provided – education, skills training, and guidance on how to change sexual behaviour – as required for coverage.
For services provided on an annual basis, this is defined as a 12-month period.
Deductible and Coinsurance
Effective for dates of service on and after November 8, 2011, deductible and coinsurance do not apply to claim lines with HCPCS code G0445.


