(2023) Modifier 59 | Distinct Procedural Service
Modifier 59 is used for Distinct Procedural Services. Multiple services provided to a patient on one day by the same provider may appear to be incorrectly coded, when in fact the services may have been performed as reported.
Because these circumstances cannot be easily identified modifier 59 was established to permit claims of such a nature to bypass correct coding edits.
The addition of this modifier to a procedure code indicates that the procedure represents a distinct procedural service from others billed on the same date of service.
In other words, this may represent a different session, different surgery, different anatomical site or organ system, separate incision/excision, different agent, different lesion, or different injury or area of injury (in extensive injuries).
Modifier 59 | Description
The CPT Manual describes Modifier 59 as follows:
“Distinct Procedural Service: Under certain circumstances, it may be necessary to indicate that a procedure or service was distinct or independent from other non-E/M services performed on the same day.
Modifier 59 is used to identify procedures/services, other than E/M services, that are not normally reported together, but are appropriate under the circumstances.
Documentation must support a different session, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same individual.
However, when another already established modifier is appropriate, it should be used rather than modifier 59.
Only if no more descriptive modifier is available, and the use of Modifier 59 best explains the circumstances, should Modifier 59 be used.”
Note: Modifier 59 should not be appended to an E/M service. To report a separate and distinct E/M service with a non-E/M service performed on the same date, see Modifier 25.
Coding Guidelines For Modifier 59
When you have distinct, separate procedures, know which modifiers will get the claim paid in full. Modifier 59 acts as a “universal unbundling” modifier for procedures that are normally included as part of another procedure, or “bundled.”
The modifier tells the payer that there are special circumstances that warrant separate reporting (and payment) of the unbundled code.
Special circumstances that generally warrant modifier 59 include;
- The procedures were performed at separate encounters on the same day;
- The procedures were performed during the same encounter on separate anatomic organ systems or body sites, incisions, excisions, lesions, or injuries;
- The procedures were timed and performed sequentially;
- The diagnostic procedure preceded and was the basis for a therapeutic procedure;
- An unplanned diagnostic procedure occurred subsequent to the therapeutic procedure.
How To Avoid Denials For Modifier 59
Because claims are processed without the physician’s documentation, payers rely on the information sent to them to be accurate and assume there is documentation backing it up. Unfortunately, modifier 59 gets misused a lot.
As a result, some payers now automatically deny CPT codes appended with modifier 59. This forces the provider to appeal the denial and send in the documentation to show that modifier 59 was applied correctly.
This denial and appeal process is costly for both the provider and the payer — it delays payment and forces the provider’s staff to write appeals and the payer’s staff to read documentation and process appeals.
Usage & Reimbursement Of The 59 Modifier
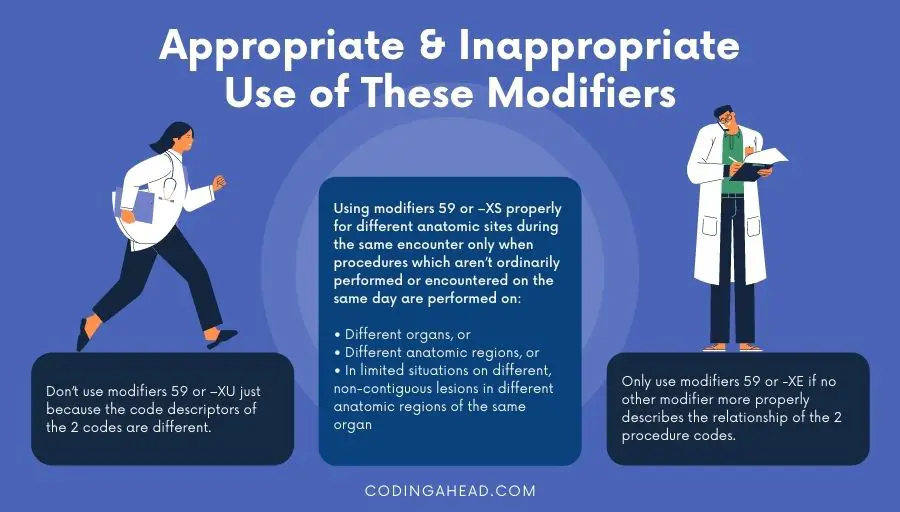
Modifier 59 is used appropriately for different anatomic sites during the same encounter only when procedures which are not ordinarily performed or encountered on the same day are performed on different organs, or different anatomic regions, or in limited situations on different, non-contiguous lesions in different anatomic regions of the same organ.
The 59 modifier is used appropriately when the procedures are performed in different encounters on the same day,
The modifier is used inappropriately if the basis for its use is that the narrative description of the two codes is different.
The 59 modifier is used appropriately for two services described by timed codes provided during the same encounter only when they are performed sequentially.
Modifier 59 is used appropriately for a diagnostic procedure which precedes a therapeutic procedure only when the diagnostic procedure is the basis for performing the therapeutic procedure.
The modifier is used appropriately for a diagnostic procedure which occurs subsequent to a completed therapeutic procedure only when the diagnostic procedure is not a common, expected, or necessary follow-up to the therapeutic procedure.
Don’t use modifier 59 with CPT 77427 (description: Radiation treatment management, five treatments) and CPT 99201 – CPT 99499 (Evaluation and management services).
When a provider submits a claim for any of these codes with Modifier 59, the carrier must process the claim as if the modifier were not present.
Examples Of Modifier 59
Underneath two billing examples of the 59 modifier.
Example 1
Modifier 59 (different substance) should be attached to the lesser valued technique indicating that separate agents were administered by different techniques.
CPT codes describing chemotherapy administration include codes for the administration of chemotherapeutic agents by multiple routes, the most common being the intravenous route.
For a given agent, only one intravenous route (push or infusion) is appropriate at a given session. It is recognized that frequently combination chemotherapy is provided by different routes at the same session.
When this is the case, using the CPT codes 96408, 96410, and 96414.
Example 2
Modifier 59 should be attached to the initial incisional hernia repair code. When a recurrent incisional or ventral hernia requires repair, the appropriate recurrent incisional or ventral hernia repair code is billed.
A code for initial incisional hernia repair is not billed in addition to the recurrent incisional or ventral hernia repair unless a medically necessary initial incisional hernia repair is performed at a different site.
X Modifiers That Have Replaced Modifier 59
The Centers for Medicare & Medicaid Services (CMS) created four modifiers, referred to as X[ESPU] Modifiers, to better differentiate between the reasons for unbundling codes,
- Modifier XE: Separate encounter
- Modifier XS: Separate structure
- Modifier XP: Separate practitioner
- Modifier XU: Unusual non-overlapping service
The X modifiers apply to Medicare Part B. Some commercial insurance companies have indicated in their online reimbursement manuals that they will process the X[ESPU] modifiers, such as Horizon Blue Cross Blue Shield of New Jersey.
CMS does not require providers to use modifiers X[ESPU] instead of modifier 59, and they continue to accept modifier 59 for now.
However, if your practice ignores the modifiers that carry more specific information and uses modifier 59 instead, do not be surprised if your Part B carrier audits your modifier 59 usage to ensure it’s not being over-utilized to unbundle CPT codes.
Be sure to review the documentation and ask yourself if the unbundling is justified enough to apply the appropriate X[ESPU] modifier.


