How To Use CPT Code 93655
Table of Contents
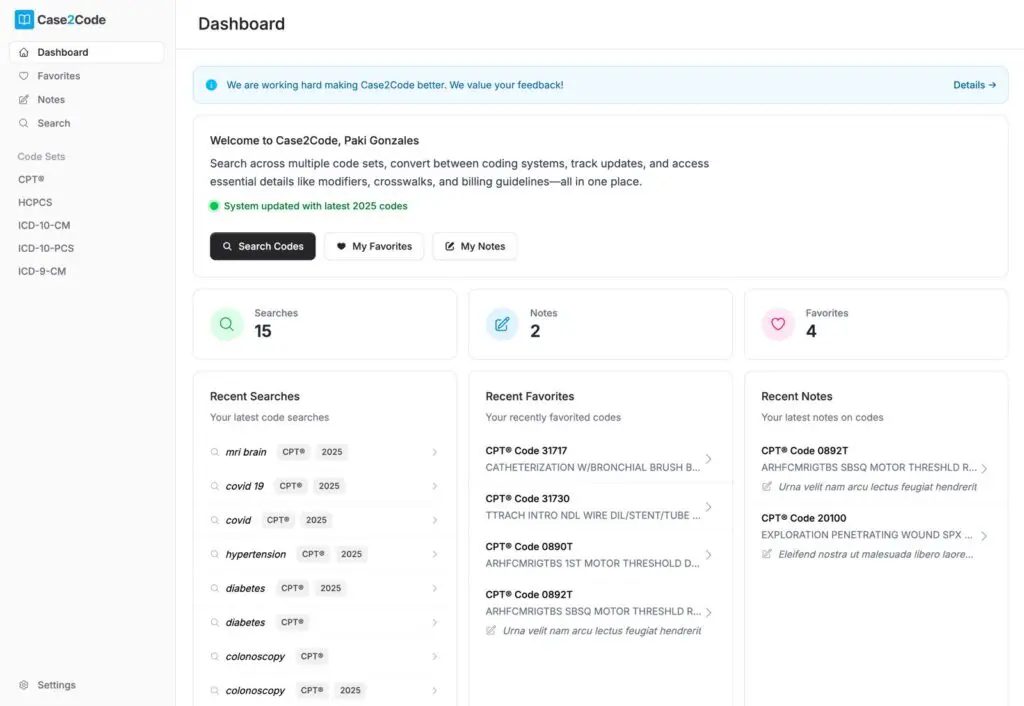
This Content Might Be Outdated – Check in Our Free Code Lookup Tool
Medical codes change frequently, and using outdated information can lead to denials. Ensure you're working with the most up-to-date version of CPT Code 93655 by opening it in our free code lookup tool.
- Instant Access to the Latest Codes
- Detailed Code Insights & Guidelines
- 100% Free to Use
CPT 93655 refers to the intracardiac catheter ablation of a discrete mechanism of arrhythmia, which is a specialized procedure aimed at treating abnormal heart rhythms. This procedure is performed after an initial ablation and involves the use of diagnostic maneuvers to identify and address additional arrhythmias that may not have been resolved by the primary ablation. By utilizing a catheter inserted through the groin, the healthcare provider can access the heart and deliver targeted radiofrequency energy to destroy the problematic tissue responsible for the arrhythmia, thereby restoring normal heart rhythm.
1. What is CPT code 93655?
CPT code 93655 represents a specific medical procedure involving the intracardiac catheter ablation of arrhythmias that are distinct from the primary ablation mechanism. This code is utilized when a healthcare provider performs additional diagnostic maneuvers to assess the heart’s electrical activity after an initial ablation procedure. The purpose of this code is to document the treatment of spontaneous or induced arrhythmias that may arise, ensuring that the provider is compensated for the additional work involved in identifying and addressing these issues. The clinical relevance of this procedure lies in its ability to improve patient outcomes by effectively managing complex arrhythmias that may not respond to standard treatment methods.
2. Qualifying Circumstances
This CPT code can be used in specific circumstances where a patient has undergone a primary ablation procedure but continues to experience arrhythmias. The criteria for using this code include the necessity for repeat diagnostic maneuvers to evaluate the heart’s electrical activity and the identification of additional arrhythmias that require intervention. It is important to note that this code should only be reported in conjunction with a primary procedure code, as it is classified as an add-on code. Inappropriate use of this code would occur if it is reported without a corresponding primary procedure or if the arrhythmias being treated do not meet the criteria for additional intervention.
3. When To Use CPT 93655
CPT 93655 is used when a healthcare provider conducts electrophysiology testing following an initial ablation procedure to assess the effectiveness of the treatment and to identify any remaining arrhythmias. This code should be reported when the provider performs additional catheter-based interventions to address these arrhythmias. It is crucial to use this code alongside the appropriate primary procedure code, as it cannot be reported independently. Additionally, providers should be aware of any restrictions regarding the use of this code in conjunction with other specific codes that may pertain to the patient’s condition or treatment plan.
4. Official Description of CPT 93655
Official Descriptor: Intracardiac catheter ablation of a discrete mechanism of arrhythmia which is distinct from the primary ablated mechanism, including repeat diagnostic maneuvers, to treat a spontaneous or induced arrhythmia (List separately in addition to code for primary procedure).
5. Clinical Application
The clinical context for CPT 93655 involves the management of complex arrhythmias that may persist after an initial ablation procedure. This procedure is critical for patients who continue to experience irregular heartbeats, as it allows for targeted treatment of specific areas within the heart that may be contributing to the abnormal rhythm. By utilizing electrophysiology testing, providers can gain valuable insights into the heart’s electrical pathways and effectively address any remaining issues, ultimately improving the patient’s quality of life and reducing the risk of complications associated with untreated arrhythmias.
5.1 Provider Responsibilities
During the procedure associated with CPT 93655, the provider is responsible for several key actions. Initially, the provider ensures that the patient is appropriately prepped and anesthetized. Following the initial ablation, the provider conducts electrophysiology testing to assess the electrical activity at multiple locations within the heart. If necessary, the provider may induce arrhythmias to pinpoint the origin of any abnormal rhythms. Once identified, the provider places a specialized catheter at the site to deliver radiofrequency energy, effectively destroying the problematic tissue. After completing the procedure, the provider carefully removes the catheters and instruments, applying pressure to the access sites to minimize bleeding.
5.2 Unique Challenges
One of the unique challenges associated with CPT 93655 is the complexity of accurately identifying the source of arrhythmias, especially in patients with multiple potential sites of abnormal electrical activity. The provider must be skilled in interpreting the results of electrophysiology testing and adept at navigating the heart’s intricate anatomy. Additionally, there may be risks associated with catheter placement and the delivery of radiofrequency energy, including potential damage to surrounding tissues or the induction of new arrhythmias. These challenges necessitate a high level of expertise and careful monitoring throughout the procedure.
5.3 Pre-Procedure Preparations
Before performing the procedure associated with CPT 93655, the provider must conduct thorough evaluations to ensure the patient’s safety and suitability for the intervention. This may include reviewing the patient’s medical history, conducting imaging studies to assess heart structure, and performing preliminary electrophysiology studies to identify existing arrhythmias. Additionally, the provider must ensure that the patient is adequately informed about the procedure, its risks, and the expected outcomes. Proper pre-procedure preparations are essential for minimizing complications and optimizing the effectiveness of the treatment.
5.4 Post-Procedure Considerations
After the procedure, the provider must monitor the patient closely for any signs of complications, such as bleeding or arrhythmias. Follow-up care may include additional electrophysiology studies to assess the success of the ablation and to determine if further interventions are necessary. The provider should also provide the patient with instructions for post-procedure care, including activity restrictions and signs of potential complications that warrant immediate medical attention. Ongoing follow-up appointments may be required to evaluate the patient’s heart rhythm and overall cardiac health.
6. Relevant Terminology
Ablation: The removal of tissue or destruction of its function, often used in the context of treating abnormal heart rhythms.
Arrhythmia: An irregular or abnormal heartbeat that can lead to various health complications.
Catheter: A flexible tube inserted into a vessel or tubular structure to allow for the passage of instruments, withdrawal of blood, or instillation of fluids.
Discrete: Referring to something that is separately identifiable or distinct from other elements.
Electrophysiology study (EPS): Tests that evaluate the electrical activity of the heart to detect abnormalities in heart rhythm.
Intracardiac: Pertaining to or occurring within the heart.
Radiofrequency ablation (RFA): A technique that uses heat generated by focused electromagnetic waves to destroy abnormal tissue or lesions.
7. Clinical Examples
1. A patient with a history of atrial fibrillation undergoes an initial ablation but continues to experience episodes of rapid heart rate. The provider performs additional testing to identify the source of these episodes.
2. After a successful ablation for ventricular tachycardia, a patient presents with new symptoms of palpitations. The provider conducts an electrophysiology study to assess the heart’s electrical pathways.
3. A patient with a complex arrhythmia profile requires repeat ablation procedures. The provider uses CPT 93655 to document the additional interventions performed.
4. Following an initial catheter ablation, a patient experiences recurrent atrial flutter. The provider performs diagnostic maneuvers to locate the arrhythmia’s origin.
5. A patient with a history of syncope undergoes an electrophysiology study after an initial ablation to evaluate for any remaining arrhythmias.
6. A healthcare provider identifies a discrete area of abnormal electrical activity during an electrophysiology study and uses radiofrequency energy to ablate it.
7. A patient with persistent atrial fibrillation undergoes a second ablation procedure, and the provider uses CPT 93655 to report the additional diagnostic testing performed.
8. After an initial successful ablation, a patient returns with symptoms of irregular heartbeat. The provider conducts further testing to determine if additional ablation is necessary.
9. A patient with a history of multiple arrhythmias undergoes a comprehensive electrophysiology study to assess the effectiveness of previous ablation treatments.
10. Following a catheter ablation for atrial fibrillation, a patient experiences new-onset palpitations, prompting the provider to perform additional diagnostic maneuvers to identify the cause.