90715 CPT Code (2023) | Description, Guidelines, Reimbursement & Example
90715 CPT code is a medical procedure code in the domain of tetanus and diphtheria toxoids. CPT 90715 may be used for young children older than seven years. A dose of this combination immunization, given to anyone seven years of age and older as a booster, prevents lockjaw, diphtheria, and whooping cough.
Summary
Vaccinations, such as anti-rabies therapy, tetanus antitoxin, or booster immunizations, are frequently not covered by Medicare unless they directly relate to treating an injury or direct exposure to a disease or condition.
Preventive immunizations (vaccination or inoculation) for smallpox, typhoid, and polio are not covered if there is no harm or direct exposure. The total cost will reject if a vaccination or immunization is not covered (such as office visits primarily for administering a non-covered injection).
If an injection may be administered to a patient who is only partially immunized, the insurance company will cover the cost. A patient should have one booster dose if they have had the primary immunization, have a high-risk wound, and have not had the vaccine within the last five years.
The patient does not have a primary vaccine, their major immunization status is uncertain, and they have a high-risk wound. In the 90715 CPT code, these injections may use: Immune globulin will cover by policy INJ-012.
When a tetanus booster may administer to a patient who will never expose to it, Medicare does not cover the cost of the injection (even though it may be an appropriate preventative treatment). Medicare should not pay for preventive care.
Specific requirements for coverage apply to each vaccination. For example, following exposure, vaccinations may cover vaccines against tetanus, diphtheria, pertussis, and tetanus-diphtheria.
These injections are covered when administered for an acute injury to a person who is only partially tetanus-immunized. Tetanus prophylaxis recommendations depend on the patient’s immunization history and the state of the wound.
The toxoid may supply more severe wounds if the patient has not received a booster dosage for five years. Conversely, tetanus toxoid may treat clean, minor injuries if the patient has not had a booster dose in the past ten years.
When more than five years have passed after receiving the last dose of the tetanus toxoid-containing vaccine, a tetanus toxoid vaccine may recommend for wound care. For those who have never gotten Tdap or whose Tdap history is unknown, Tdap may prefer when a tetanus toxoid-containing vaccine may recommend for people under 11.
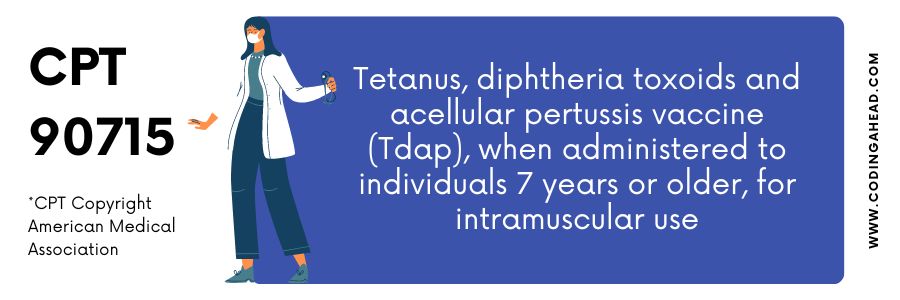
Description Of The 90715 CPT Code
Under this code, only children under seven may be entitled to reimbursement.
The official description of CPT code 90715 is: “Tetanus, diphtheria toxoids and acellular pertussis vaccine (Tdap), when administered to individuals 7 years or older, for intramuscular use.”
An Advance Beneficiary Notice can deliver to a patient after a doctor administers a Tetanus or Td/DT vaccine (ABN). Providers and services must present patients with an Advance Beneficiary Notice (Modifier SL) before submitting claims to Medicare (ABN).
You may submit more than one unit of code 90715 for each first dosage of vaccination or toxoid. Therefore, there should be no need to make any changes if more than one first component may report.
Also, remember that the 90715 CPT code covers single-component immunizations and combo vaccinations (such as influenza, human papillomavirus, or pneumococcal conjugate vaccines).
This base code may record for each vaccine that a patient under 18 receives vaccination advice from a doctor or other competent health care practitioner. The 90461 add-on code may use for each additional vaccination component t
Billing Guidelines
Only individuals requiring treatment for an injury are eligible for tetanus immunization under the Medicare Part B program (and additional tetanus vaccines that include diphtheria or pertussis components).
Part B, for example, would cover the immunization and administration costs if the recipient required a tetanus injection due to an unintentional puncture.
If a beneficiary requires a tetanus booster dosage for a reason other than an accident or illness, the vaccination and administration code will reject non-covered. Therefore, beneficiaries should contact their Medicare Part D plan to determine coverage.
Medicare covers the cost of the discarded drug or biological residue in a single-use product after administering the reasonable and necessary dosage.
Suppose the doctor has taken good-faith steps to reduce the unused portion of the medicine or biological by how it will supply, how patients may schedule, and how it is ordered, accepted, preserved, and used. In that case, Medicare will cover the amount discarded and delivered.
Pneumococcal vaccination CPT codes include the following:
- Both 90670 and 90732 pay roughly $108 per hour, respectively.
- The TDAP vaccine is covered by CPT code 90715 (about $31).
Remember that Medicare periodically modifies payment information, including influenza vaccine coverage.
When vaccines may deliver as part of a well-child visit, ICD 10 suggests that codes Z00.121 or Z00.129 (regular health check for children over 298 days old) include immunizations relevant to the patient’s age.
Examples
A young lady around eleven comes in for a checkup. The mother has signed formal consent for immunizations. It’s also essential for a doctor to explain to a child and her mother why they should get vaccinated against HPV, Tdap, and seasonal influenza (90715). The doctor keeps a record of the discussion.
Then, one of the nurses administers the vaccinations to the patient, ensures that it is properly recorded, and monitors the patient for any immediate side effects.
The procedure described by the 90715 CPT code is administered so this code can be billed.




