99222 CPT Code (2023) – Description, Guidelines, Reimbursement, Modifiers & Examples
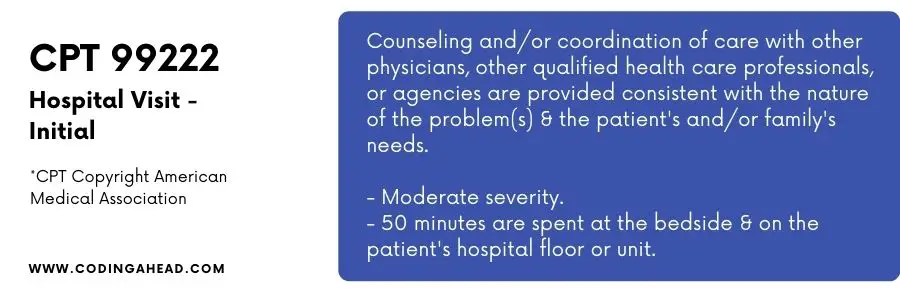
99222 CPT code describes the initial hospital care visit of moderate complexity.
Before admitting a patient into in-patient settings, the admitting physician may execute an evaluation and management encounter.
Moreover, all the critical components of an E&M service, e.g., history, exam, and medical decision making, are inclusive.
Only a qualified physician can carry out all three key elements, as per the CMS guidelines stated for initial visits.
99222 CPT code presents the history and exam as comprehensive and the Medical decision making as moderate complexity.
The coders should pay appropriate attention while coding an evaluation and management chart of the initial in-patient visit based on those as mentioned earlier three key components.
All of the above mentioned vital components must be present in a note. Because if any of the components or subcomponents is missing, it may lead directly to a low-level code selection.
Although the new evaluation and management guidelines are not applicable in in-patient settings, time spent with patients or families at the bedside or the hospital floor is considered a key factor.
For this level of E&M code, typically, 50 minutes are spent face to face with the patient or with the caregiver/family.
99222 CPT Code | Description
CPT code 99222 is a mid-level service code concerning the severity order of initial in-patient provider encounters.
The other two codes which fall in this category are CPT 99221 and CPT 99223.
CPT 99221 presents the lowest severity, and CPT 99223 offers the highest severity encounter. All three key components are crucial for appropriate level code selection.
If any critical components were not performed or not available in the medical chart, it might result in payment losses.
The history of a medical chart must include the below components:
Component 1: History
- History of present illness
- Review of systems
- Past Family and social history
The provider must mention the chief complaints in the history of present illness concerning location, timing, context, duration, quality, modifying factors, and associated signs and symptoms.
Review of the system consists of provider interrogations to count the body systems to identify signs and symptoms the patient has experienced or is currently experiencing.
This comprehensive analysis of systems assists the provider in finding any changes in the patient’s body, which will help further identify any problems in the initial stages.
The system review generally consists of questions that a patient can answer.
The physician can mark it as yes or no. In this portion, the patient tells the physician about his general health.
Review of the system should be confused with examination as both portions are similar but used for different purposes in an evaluation and management chart.
The complete systems included in the systematic review are general symptoms, for example, eyes, ears, nose, mouth, and throat (ENMT), Cardiovascular (CV), Respiratory, Gastrointestinal (GI), Genitourinary (GU), Musculoskeletal (MS), Skin (Integumentary), Neurological, Psychiatric, Endocrine, Blood-related disorders (Hematology or lymphatic), allergic.
Component 2: Examination
This portion of history follows two different documentation guidelines called 1995 and 1997.
The difference between these guidelines is the assessment methodology.
The 1995 guidelines describe the examination by the body area, i.e., head, neck, chest, abdomen, genitalia, back, and extremities.
On the other hand, the 1997 guidelines recognize the organ system, i.e., respiratory, cardiovascular, eyes, skin, etc.
By both methods, the coder can select the appropriate level of examination.
The provider evaluates these systems one by one. He can determine one system in detail as per the patient’s condition.
Component 3: Medical Decision Making
Medical decision-making is the most critical part of the three components of evaluation and management.
It narrates the nature of presenting problem, the medical necessity of the encounter, and any new crisis that may add the highest scores in the overall MDM chart.
Data review and treatment options also contain higher weights in the final calculation to present the optimal evaluation and management in initial encounters.
So based on the above three key elements, a final level of E&M is selected to present the severity of an encounter.
Review of complete details in a medical chart is critical for appropriate CPT code selection.
Billing Guidelines
The POS (place of service) for CPT 99222 should be presented as IH while billing, as the provider can only perform this service in in-patient settings.
The same specialty provider can execute this service only once per day. Suppose the provider needs consultation from a different specialty.
In that case, the coder codes the claim separately for the physician furnishing the consultation request.
The insurances govern the payment schedule, but as most commercial insurances do not accept the consultation codes, the coder should submit encounters as an initial in-patient evaluation and management.
If a provider accomplished only his part in a service, he might get a split share visit by an NPP, and the coder may bill it under the provider’s NPI.
The split share visits are not acceptable unless supervised and signed by the resident treating physician.
The documentation should indicate two separate portions of the treating physician and NPP personally performed.
While billing for in-patient encounters, the coder or biller must consider the same-day admission and discharge scenarios.
If the patient gets admission and discharged on the same day, the coder must bill the assessment meeting with different E&M codes.
In such cases billing initial in-patient and discharge codes separately in a single claim or multiple claims is not justifiable as per the AMA coding manual.
Reimbursement
The provider carries out initial in-patient evaluation and management code selection with the help of the three components of the medical chart above.
So, to avoid over or under coding of an encounter, the provider should mention complete details of the meeting.
However, the time of encounter is essential to determine the level.
If the time is not reasonable by the points mentioned in the medical chart, the insurance may not prefer this claim.
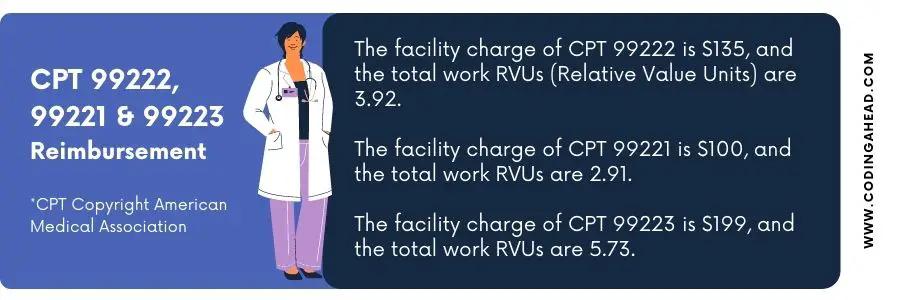
The facility charge of CPT 99222 is $135, and the total work RVUs (Relative Value Units) are 3.92.
The facility charge of CPT 99221 is $100, and the total work RVUs are 2.91.
The facility charge of CPT 99223 is $199, and the total work RVUs are 5.73.
The evaluation and management service charges may vary as per the contractual obligation of individual insurance.
CPT 99222 Modifiers
There are only a limited number of modifiers allowed with CPT code 99222. Each of the modifiers is explained below in detail.
The coder should be attentive while appending these modifiers with CPT code 99222 because their misuse or overuse can lead to comprehensive audits.
If these modifiers are not present in a claim when required, the provider may not get any reimbursements.
Following are the practical examples and applications of modifiers 24, 25, 57:
Modifier 24
Append modifier 24 with CPT 99222 in a case when the initial in-patient visit falls in the global period of any previously performed major or minor surgical procedure.
The global period divides into 10 – days or 90 – days, depending on the complexity of the process.
For example, all the major surgical procedures must have a global period of 90 – days, such as nephrectomy.
At the same time, all the minor surgical procedures must have a global period of 10 – days, for instance, incision and drainage of abscess from the left arm.
Suppose the patient receives any initial in-patient evaluation and management service during that global period. In that case, submit the claim with modifier 24.
Another rule governing this scenario is that if a provider accomplishes any major or minor surgical procedure having a global period, the encounter should be different concerning the reason.
Modifier 57
Append Modifier 57 as a principal modifier with CPT 99222; in this case, the provider decides for surgery on the initial evaluation and management day.
It shows that it also includes a day before surgery in the global surgical package for minor and major surgical procedures. And the covering companies may not reimburse it separately.
Modifier 25 is the most common modifier used with evaluation and management codes.
Use this modifier with an E&M code when the physician executes a separately identifiable service on the day of the encounter.
For example, minor surgical procedures have no global period, i.e., TB testing, EKG monitoring, etc.
And modifier 25 will make the E&M service eligible for payments.
Suppose, if someone does not use modifier 25, the insurance may consider E&M inclusive into the other service performed on the same day.
Modifier AI
Modifier AI is used with the primary admitting physician CPT code in a case when a provider from any other specialty provides consultation on request of admitting physician.
Medicare accepts the consultation codes, but most commercial insurances do not agree with the consultation CPT codes.
As a policy, they direct the practices to use the alternate initial in-patient evaluation and management codes to get reimbursements.
In such cases, the AI modifier differentiates the principal physician from the consulting physician and makes a claim eligible for refunds.
Suppose a physician provides services in unlisted health professional shortage area.
In that case, he must append modifier AQ to get reimbursed at higher rates.
As per the government policy, insurance companies reimburse the services in rural areas at a higher rate than in urban areas.
Telehealth Modifiers
Telehealth modifiers such as 95 and GT are also applicable with CPT code 99222 in a case when the physician provides the service as a telehealth visit. Such visits are more common in rural areas or when there is a public health emergency, such as during the Covid 19 crisis.
The place of service will be IH; only the modifier will differentiate and presents the mode by which the provider furnishes the service.
Selecting appropriate modifiers per the situation requirements is the key to timely reimbursements.
Most of the modifiers mentioned earlier are applicable in the eligible payment category.
Failure to append those modifiers in a claim will result in a denial.
Difference Between CPT 99221 & 99222
The key difference between medical CPT code 99221 and 99222 is severity.
In CPT code 99221, the severity of hospitalisation is comparably low, while the severity of medical hospitalisation in CPT code 99222 is fairly high.
Another comparison to note for CPT 99221 and CPT 99222 is that in the case of CPT 99221, doctors typically spend 30 minutes with the patient at the patient’s bed and floor unit, however in CPT 99222, doctors typically spend 50 minutes with a patient at the patient’s bed and floor.
The times are recorded for each service in the CPT manual as a guide only. Time plays a huge role when it comes to determining time-based CPT coding.
Times are generally listed for each service in the CPT manual. CPT lists a number of CPT codes that are very time-dependent and even have long service codes.
This normally creates general confusion about time-based coding, in particularly when medically coding inpatient visits and unusually long outpatient visits.
This is known as time-based medical coding.
With the appropriate understanding of time and its relation to coding, clinicians can make an knowledgable decision while deciding the patient’s code, although medical history, examination, and decision elements lack total data and details.
Time-based medical coding helps doctors better resolve situations and make thought-out decisions along with available data sets.
Examples of CPT 99222
The following are examples of when CPT code 99222 may be used.
Example 1
A 67 years old patient suffering from acute appendicitis came for a check-up.
Dr. Smith admitted the patient to a hospital to monitor the patient’s condition and for further interventions.
The admitting physician calls in a GI surgeon for consultation.
Then the physician started treatment immediately with IV antibiotics and pain killers — the patient’s insurance in Medicare.
Dr. Smith admits a patient in the above example, so the coder must bill an initial in-patient visit CPT 99222 under Dr. Smith’s NPI. Dr. Smith called for a consultation by a GI specialist.
The coder should now bill another initial in-patient E&M code under consulting Dr. NPI on the same DOS (date of service).
The patient’s health insurance is Medicare, and it does not accept the consultation CPT codes.
Suppose the coder does not use modifier AI with the principle admitting physician’s E&M CPT code.
In that case, the covering companies may deny both claims because the insurance does not get notified about the consultation on the same day.
Example 2
A 70 years old male comes into the hospital with acute tonsillitis, chest pain, and high-grade fever.
The patient’s condition is deteriorating with time. He had a nephrectomy procedure 3 – weeks ago in the same hospital due to a benign tumor in his left kidney.
It is evident that the patient’s visit is because of new symptoms and has no correlation with the previous procedure.
The physician performs an initial in-patient evaluation and admits the patient for further treatment and monitoring of the patient’s condition.
In the above example, the patient is already in the global period of a major surgical procedure of 90 – days.
Still, the reason for this encounter is unrelated to the reason for the surgery.
In cases when the specialty is different, the encounter will be considered an initial in-patient encounter.
In this case, append modifier 24 with the CPT 99222. Keep the diagnosis for acute tonsillitis at a primary position with CPT 99222.
However, the encounter does not relate to the previous surgical procedure.
Example 3
A 25 – years old male came into the hospital with a high-grade fever, pain, chills, generalized body weakness, and an abscess on his right arm.
The physician performed an initial in-patient evaluation and management and decided to perform incision and drainage of the bump on the same day of the encounter.
In the above example, the physician decided for surgery on the same day as of initial in-patient evaluation.
Append modifier 57 with the CPT 99222 because I&D (Incision and Drainage) is a minor surgical procedure.
I&D has a global period of 10 – days. The provider performs an E&M on the same day of surgery.
It is a part of the procedure thus will not reimburse separately on the day of surgery.
More Examples
Example 4
Initial hospital visit for a 50-year-old patient with lower quadrant abdominal pain and increased temperature, but without septic picture. (General Surgery/Abdominal Surgery/Colon & Rectal Surgery)
Example 5
Initial hospital visit for airway management, due to a benign laryngeal mass. (Otolaryngology/Head & Neck Surgery)
Example 6
Initial hospital visit for a 66-year-old female with an L-2 vertebral compression fracture with acute onset of paralytic ileus; seen in the office two days previously. (Orthopaedic Surgery)
Example 7
Initial hospital visit and evaluation of a 15-year-old male admitted with peritonsillar abscess or cellulitis requiring intravenous antibiotic therapy/ (Otolaryngology/Head & Neck Surgery)
Example 8
Initial hospital visit for a 42-year-old male with vertebral compression fracture following a motor vehicle accident. (Orthopaedic Surgery)
Example 9
Initial hospital visit for a patient with generalized atopic dermatitis and secondary infection. (Dermatology)
Example 10
Initial hospital visit for a 3-year-old patient with high temperature, limp, and painful hip motion of 18 hours’ duration, (Pediatrics/Orthopaedic Surgery)
Example 11
Initial hospital visit for a young adult, presenting with an acute asthma attack unresponsive to outpatient therapy. (Allergy & Immunology)
Example 12
Initial hospital visit for an 18-year-old male who has suppurative sialadenitis and dehydration. (Oral & Maxillofacial Surgery)
Example 13
Initial hospital visit for a 65-year-old female for acute onset of thrombotic cerebrovascular accident with contralateral paralysis and aphasia. (Neurology)
Example 14
Initial hospital visit for a 50-year-old male chronic paraplegic patient with pain and spasm below the lesion. (Anesthesiology)
Example 15
Partial hospital admission for an adolescent patient from chaotic blended family, transferred from inpatient setting, for continued treatment to control symptomatic expressions of hostility and depression. (Psychiatry)
Example 16
Initial hospital visit for a 15-year-old male with acute status asthmaticus, unresponsive to outpatient therapy. (Internal Medicine)
Example 17
Initial hospital visit for a 61-year-old male with history of previous myocardial infarction, who now complains of chest pain. (Internal Medicine)
Example 18
Initial hospital visit of a 15-year-old on medications for a sore throat over the last two weeks, The sore throat has worsened and patient now has dysphagia, The exam shows large necrotic tonsils with an adequate airway and small palpable nodes. The Initial mono test was negative. (Otolaryngology/Head & Neck Surgery)
Example 19
Initial hospital evaluation of a 23-year-old allergy patient admitted with eyelid edema and pain on fifth day of oral antibiotic therapy. (Otolaryngology/Head & Neck Surgery)
Example 20
Hospital admission, young adult pain, failed previous therapy and now present in acute asthmatic attack. (Family Medicine/Allergy & Immunology)
Example 21
Hospital admission of a 62-year-old smoker, established patient, with bronchitis in acute respiratory distress. (Internal Medicine/Pulmonary Medicine)
Example 22
Hospital admission, examination, and initiation of a treatment program for a 65-year-old female with new onset of right-side paralysis and aphasia. (Neurology)
Example 23
Hospital admission, examination, and initiation of treatment program for a 66-year-old chronic hemodialysis patient with fever and a new pulmonary infiltrate. (Nephrology)
Example 24
Hospital admission for an 8-year-old febrile patient with chronic sinusitis and severe headache, unresponsive to oral antibiotics. (Allergy & Immunology)
Example 25
Hospital admission for a 40-year-old male with sub maxillary cellulitis and trismus from infected lower moral. (Oral & Maxillofacial Surgery)



