A Guide to Bacterial Gastrointestinal Infections
Below we cover seven types of Bacterial Gastrointestinal Infections. Namely; Enteropathogenic Escherichia coli infection (EPEC), Enterotoxigenic Escherichia coli infection (ETEC), Enteroinvasive Escherichia coli infection (EIEC), Enterohemorrhagic Escherichia coli infection (EHEC), Campylobacter enteritis, Enteritis due to Yersinia enterocolitica, and Enterocolitis due to Clostridium difficile.
1. Enteropathogenic Escherichia coli infection (EPEC)
Enteropathogenic Escherichia coli, also known as EPEC and typically ingested with contaminated water and food, adhere to the epithelial lining of the intestines and cause gastroenteritis and severe diarrhea in infants and children less than one-year-old, particularly in developing countries.
EPEC carries multiple virulence factors, including the adherence factor, which causes an inflammatory response but does not produce a heat-labile toxin (LT) and heat stable toxin (ST), virulence factors associated with the bacteria. EPEC can affect adults, but it takes a considerable amount of bacteria.
1.1 Symptoms
A patient with EPEC infection can experience;
- severe, sometimes bloody diarrhea;
- stomach pain;
- fever;
- (in severe cases) the patient may become highly dehydrated; and
- children may develop seizures.
1.2 Diagnosis
Laboratory tests of the patient’s feces can detect the bacterium, and culture and sensitivity can identify the most effective antibiotic(s).
1.3 Treatment
Treatment includes rehydration with oral or intravenous fluids and, in severe cases, antibiotics; less severe cases generally resolve without antibiotics.
2. Enterotoxigenic Escherichia coli infection (ETEC)
The bacterium Enterotoxigenic Escherichia coli, also known as ETEC and typically ingested with contaminated water and food, causes a form of gastroenteritis commonly referred to as traveler’s diarrhea.
They do not produce inflammation in the intestines. ETEC produces heat-labile toxin (LT) and heat-stable toxin (ST), virulence factors associated with the bacteria.
2.1 Symptoms
EPEC infection is usually self–limiting. A patient with EPEC infection can experience;
- “rice–water” diarrhea without fever or only slight fever;
- stomach pains; and
- loss of appetite.
Children and adults with compromised immune symptoms may experience more severe symptoms over an extended period.
2.2 Diagnosis
Laboratory tests of the patient’s stools can detect the E. coli bacterium.
2.3 Treatment
EPEC generally resolves independently, but treatment can include antibiotics, rehydration, and sometimes hospitalization in severe cases.
3. Enteroinvasive Escherichia coli infection (EIEC)
Enteroinvasive Escherichia coli, also known as EIEC and typically ingested with contaminated water and food, causes a mild form of dysentery similar to that caused by Shigella.
EIEC does not produce heat-labile toxin (LT) and heat-stable toxin (ST), virulence factors associated with the bacteria.
3.1 Symptoms
A patient with EIEC infection experiences;
- mild dysentery symptoms;
- watery diarrhea, sometimes containing blood and mucus;
- fever;
- chills;
- vomiting;
- stomach pains;
- and loss of appetite.
3.2 Diagnosis
Laboratory tests of the patient’s stools can detect the E. coli bacterium.
3.3 Treatment
EIEC generally resolves without treatment in healthy individuals, but children and those with compromised immune systems may require antibiotics and, in severe cases, rehydration and sometimes hospitalization.
4. Enterohemorrhagic Escherichia coli infection (EHEC)
The bacterium Enterohemorrhagic Escherichia coli, also known as EHEC and typically ingested with contaminated water and food, causes a severe gastrointestinal infection.
EHEC, a subset of–toxigenic E. coli (STEC), does not produce heat-labile toxin (LT) and heat stable toxin (ST) but does produce Shiga toxin, a virulence factor associated with hemolytic–uremic syndrome.
4.1 Symptoms
Healthy patients with EHEC may be pretty asymptomatic. However, EHEC can cause symptoms ranging from mild diarrhea to hemorrhagic colitis (HC), with severe abdominal cramps and bloody diarrhea.
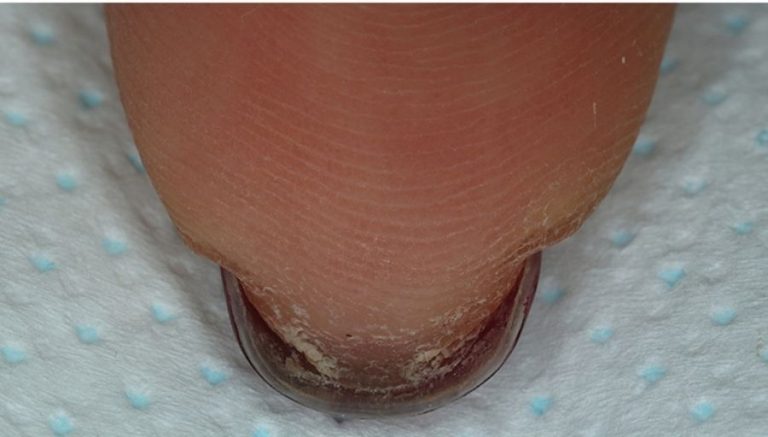
In severe cases (those caused by strains that produce Shiga toxin), the patient may become highly dehydrated and even develop life–threatening or thrombotic thrombocytopenic purpura (TTP) and hemolytic–uremic syndrome (HUS), which are characterized by anemia due to the destruction of red blood cells (hemolysis), renal failure (uremia), and ecchymoses or purpura (small bluish-purple spots due to leaking vessels under the skin).
4.2 Diagnosis
Laboratory tests of the patient’s feces can detect the bacterium, and culture and sensitivity can identify the most effective antibiotic(s). Specific amplification techniques may be used to classify virulent strains.
4.3 Treatment
Treatment includes rehydration with oral or intravenous fluids and, in severe cases, antibiotics and hospitalization.
5. Campylobacter enteritis
The bacterium Campylobacter jejuni, typically ingested with contaminated water and food, causes approximately 80% of Campylobacter enteritis (inflammation of the intestines); C. coli and C. fetus, associated with contact with animals, are less common. Campylobacter is one of the top five pathogens causing foodborne illnesses in the U.S.
5.1 Symptoms
Children under five years old and individuals between the ages of 15 and 29 are more likely to get Campylobacter enteritis than others. A patient with Campylobacter enteritis can experience;
- fever, stomach pains;
- nausea;
- vomiting; and sometimes
- watery or bloody diarrhea.
5.2 Diagnosis
Laboratory tests of the patient’s stools and blood samples can detect the bacteria.
5.3 Treatment
In healthy individuals, symptoms often resolve without treatment. Others may require antibiotics, rehydration, and, in severe cases, hospitalization.
6. Enteritis due to Yersinia enterocolitica
Yersinia enterocolitica and, less commonly, Y. pseudotuberculosis cause enteritis (inflammation of the intestines).
Foods associated with Yersinia enteritis include undercooked pork, “raw” (unpasteurized) milk, and oysters; failure to wash hands after a bowel movement or after handling contaminated food can also spread the disease.
6.1 Symptoms
Children, the elderly, and those with weakened immune systems are most at risk for acquiring Yersinia enteritis. A patient with Yersinia enteritis can experience;
- fever, stomach pains;
- nausea;
- vomiting; and sometimes
- watery or bloody diarrhea.
Some patients experience arthritis–like symptoms that can be slow to resolve.
6.2 Diagnosis
Laboratory tests of the patient’s stools and blood samples can detect the bacteria.
6.3 Treatment
Mild cases in healthy individuals usually resolve without treatment. For others, treatment includes antibiotics, rehydration, and, in severe cases, hospitalization.
7. Enterocolitis due to Clostridium difficile
Enterocolitis (inflammation of the large intestines) due to Clostridium difficile (C. diff) occurs primarily in healthcare environments where the bacteria multiply in the colon due to prolonged antibiotic therapy, killing off the “good” bacteria. C. diff can be spread from feces to food when individuals fail to wash their hands after bowel movements.
Clostridium difficile is usually present in the gastrointestinal tract of babies and young people but less so in adults; the elderly are more susceptible to infection with this bacteria.
7.1 Symptoms
A patient with C. diff enterocolitis can experience;
- watery diarrhea (sometimes containing blood or mucus);
- abdominal cramps;
- fever; and
- fatigue.
Extreme but rare symptoms include;
- colon perforation (a hole in the colon wall);
- sepsis (infection in the blood); and
- peritonitis (inflammation of the lining of the abdomen).
7.2 Diagnosis
Laboratory tests of the patient’s feces can detect the bacterium, and flexible sigmoidoscopy or colonoscopy can identify inflammatory changes or colon perforation.
7.3 Treatment
Treatment includes stopping any antibiotics the patient may receive, if possible, and rehydration with oral or intravenous fluids, different antibiotics such as metronidazole or vancomycin, probiotics, and surgery in case of complication or intestinal perforation.
Providers may educate patients on disease prevention by washing hands before consuming food and eating clean and properly cooked food.