(2023) Modifier 96 | Description, Uses, Guidelines & Examples
Modifier 96 appends with the services when the physician performs Habilitative services. Read on to find out more about what modifier 96 is and when to use it.
Description Of The Modifier 96
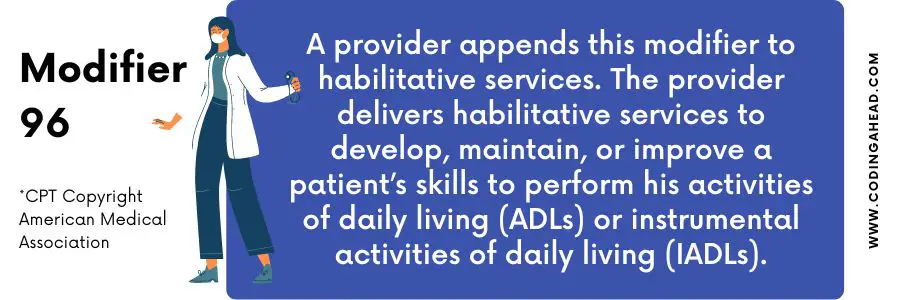
Modifier 96 indicates the services when the physician or other skilled or qualified professional offers habilitative and rehabilitative procedures or services for habilitative services in nature.
The official description of modifier 96 is: “Habilitative Services.”
The two new modifiers presented in the AMA CPT code book 2018 classify the habilitative and rehabilitative services. The following are the characteristics of modifier 96 or modifier 97 when applied to the procedure or services:
Modifier 96 applies to the service that is either habilitative or rehabilitative. The intent of this service must be habilitative.
In contrast, Modifier 97 applies to either habilitative or rehabilitative service. But the purpose of this rehabilitative.
Modifier 96 services support the induvial in learning new skills and daily routine functioning and keep enhancing these skills of the patients or individual.
In contrast, modifier 97 services support the induvial in learning new skills and daily routine functioning and keep enhancing these skills of the patients or individuals already lost or impaired because the patient was sick, disabled, or hurt.
The intent is to identify the difference between habilitative and rehabilitative services. According to the Patient Protection and Affordable Care Act (PPACA), these two modifiers must require for these services and procedures. These service helps to restore or develop the function they did not have earlier or lost due to impairment or injury.
Modifier 96 is inappropriate for bills for the service unless it supports the patient to improve the skills or functions they did not have prior. Modifier 97 is appropriate to report with physical therapy services. Documentation not supporting the services will lead to fraud and allegations during the audit review.
The insurance CareFirst may require an official statement when they are billing modifier 96 for habilitative and rehabilitative services.
CMS deleted the modifier SZ from the AMA CPT code with the replacement modifiers 96 and 97. They may require modifiers 96 or 97 for rehabilitation, physical medicines, and CPT codes.
It makes the process efficient for distinguishing habilitative from rehabilitative services.
What Is Modifier 96?
Modifier 96 applies to the services or procedures when the physician or other skilled professional provides either habilitative or rehabilitative services for the habilitative intent.
When To Use Modifier 96
The following is the use of modifier 96 when applied to the service or procedure:
The physician or other skilled professional providing the service or approach must either be habilitative or rehabilitative for habilitative services.
The Habilitative services aid an individual in learning new skills and functioning daily routine that may not adopt yet and keep learning and improving these skills.
Billing Guidelines
The Affordable Care Act (ACA) did not specify the coverage plans and terms, but they need coverage of certain essential health benefits (EHBs). This EHB includes habilitative and rehabilitative services necessary at the claim’s submission. The coverage plan may vary from State to State. One plan in one State may not be part of the coverage plan in the other.
The following two modifiers, 96 and 97, are required for the service performed on Jan 1, 2018, and after this service date when the physician reports these types of services, such as physical therapy (Habilitative and Rehabilitative Services). These services may require modifiers 96 or 97 to bill and deny them without these modifiers.
The appropriate HCPCS or CPT codes require essential modifier 96 when paying the insurance to classify the rehabilitative services. In contrast, The proper HCPCS or CPT codes require suitable modifier 97 when the bill to the insurance for rehabilitative services.
Modifiers 96 and 97 are inappropriate for bills on the same claim line when submitting to the Habilitative and Rehabilitative Services insurance.
If these claims submit with both these modifiers, they will deny by the insurance or rejected as unprocessable for Habilitative and Rehabilitative Services.
The requirements may vary for these modifiers 96 and 97 from insurance to insurance, but the following are the critical requirement when these modifiers submit to the insurance:
The physician intends to perform the therapy to improve or restore body function, which may lose due to injury, illness, acute disease, and any congenital abnormalities for Rehabilitative devices or procedures. The insurance may consider only this service when there are chances of improvements within the defined and reasonable time frame. The therapy without any modification may deny by the insurance.
The habilitative services aim to develop or maintain the skills when patients have to perform Instrumental activities of daily living (IADLs) or The activities of daily living (ADLs). They risk losing some routine functions, or the body may not develop any improvements.
The insurance may only pay for habilitative services when there is the possibility that therapy may restore bodily function or maintain routine activity due to illness (including developmental delay, congenital abnormality, or loss of a body part.
Modifier 96 and 97 Humana
According to Humana policy guidelines, modifiers 96 and 97 must append to habilitative and rehabilitative services. The requirement only applies to the beneficiary when they have separate plans for these services that lead to essential health benefits.
These requirements may have included benefits such as cognitive therapy, Physical therapy, occupational therapy, audiology, spinal manipulations, and adjustments and speech therapies. It may vary by the State and the patient’s benefit plan.
The following are the guidelines when the claim process to Humana insurance:
The service may require modifier 96 or 97 for habilitative and rehabilitative services.
They reimburse according to the benefits plan when modifier 96 or 97 attach appropriately.
It is denied by Humana insurance if both 96 and 97 bills are on the same line.
Modifiers 96 or 97 do not apply for the service other than the habilitative and rehabilitative services.
Documentation must support that modifier 96 or 97 is billed appropriately.
Other modifiers such as 59, CO, CQ, GO, GP, and GM are appropriate to report with modifiers 96 or 97 on the same line.
Billing Examples
The following are examples of when modifier 96 is applicable with CPT or HCPCS codes:
Example 1
The patient may have mobility issues, and an address by the physical therapist to improve the gait, posture correction, walking by self, and enhancing the range of motion. He may use devices or physical exercise to maintain these functions.
The mobility issues may arise from conditions such as children suffering from congenital malformations, down syndrome, cerebral palsy, etc., or physical disabilities.
A 6-year-old male child and his parent were present in a hospital outpatient setting. The child has cerebral palsy. The child is suffering from physical disabilities and cannot maintain his daily routine activities.
The physical therapist applies several sessions to the patient to improve the mobility issues of the child. The child has been able to walk with improvement in posture. It is appropriate to report this habilitative service with modifier 96.
Example 2
The patient suffers from difficulties in daily living, such as children with poor hands and eye coordination to perform a specific task. The occupational therapist may utilize different activities to improve the coordination of routine workouts, such as feeding oneself, grasping objects and handwriting, preparing meals, drinking water or tying shoe laces, etc.
The children may have genetic problems, Autism, or mental disabilities, etc. may require habilitation services to perform the daily routine task. The occupational therapist may use various techniques to improve these skills.
An eight-year-old male child presents with no other past medical or family history to the occupational therapist with cognitive disabilities. He has genetic problems and is unable to hold things in his hands. The OT provides several sessions to the children to improve their hand abilities.
The OT uses different objects and exercises to enhance the skills, such as small objects with little weights, and provides training to grab the thing. Modifier 96 is appropriate to report with OT services and check the insurance policy if these services are covered.
Example 3
The patient may have a communication problem and require a speech therapist to improve communication. Children with down syndrome or Autism can take habilitation services for language stimulation, articulation therapy, and social skills therapy.
The patient may have no physical disabilities but have a communication problem in conditions like Autotism child has communication delays, anxiety, etc. The speech therapist may require various techniques or methods to enhance communication skills.
A 9 year-old-male child presents to the speech-language pathologist therapist (SLP) with a communication problem, cannot pronounce the words correctly, and faces communication delays. The SLP provides multiple sessions to improve the communication skills of children who have Autism.
The physician trained ten words in each session with the children. He can speak approximately seven words in each session. The SLP service must report with modifier 96 to improve the habilitative service communication. The service should check before submission if the service is covered or not.
If the children have no improvements in communication problems during a particular time, it may cause a denial of the claim.




