(2023) 93015 CPT Code | Description, Guidelines, Reimbursement & Billing Example
93015 CPT code may be used when physicians perform Cardiovascular stress tests with different techniques.
Description of the 93015 CPT code
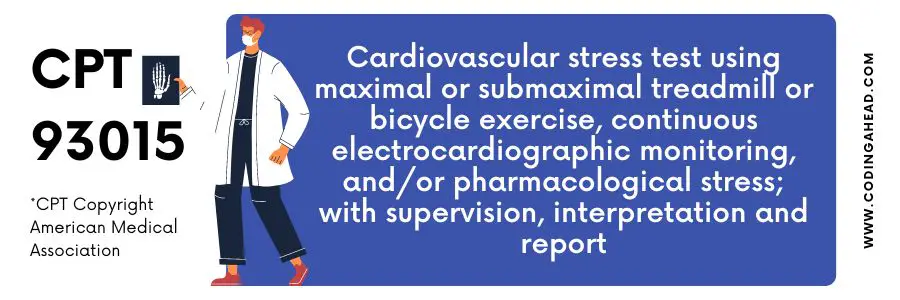
The official description of CPT code 93015 is: “Cardiovascular stress test using maximal or submaximal treadmill or bicycle exercise, continuous electrocardiographic monitoring, and/or pharmacological stress; with supervision, interpretation and report.”
The techniques included in CPT code 93015 are:
- A maximal or submaximal treadmill or bicycle exercise;
- Continuous electrocardiographic monitoring and
- Pharmacological stress.
CPT 93015 aids in identifying heart-related diseases and other conditions, such as;
- Congestive heart failure
- Heart valve disease
- Congenital heart disease
- Hypertrophic cardiomyopathy and coronary artery disease
- Angina
- Shortness of breath (dyspnea)
- Arrhythmia
- Dizziness or Lightheadedness
Physician supervised heart stress test. The test monitors the heart rhythm by electrocardiogram (ECG or EKG) during exercise (treadmill or bicycle). Drugs are administered to the patient to stimulate stress.
The physician continuously records the heart’s electrical activity acquired by an assistant supervised by a qualified health care professional. It aids in monitoring the stress on the heart.
The 93015 CPT code includes all the supervision, interpretation, and test. In contrast, CPT 93016, 93017, and 93018 include management of the test, performing of test only, and understanding of priorly performed test, respectively.
Billing Guidelines & Reimbursement
A maximum of one unit can be billed on the same CPT 93015-93018 service date. In contrast, the three units allow documentation supporting the service’s medical necessity.
The cost and RUVS of 93015 CPT code are $80.96 and 2.33960 when performed in the facility. In contrast, the reimbursement and RUVS of CPT code 93015 are $80.96 and 2.33960 when performed in the non-facility.
Some physical therapists specializing in the area of cardiopulmonary care administer maximum graded exercise tests, rehabilitate acutely ill patients in the intensive care unit, design exercise programs to restore endurance and function for patients with organ transplants, and enable patients with acute and chronic heart or lung problems to resume functional activities.
Some programs require a team of specialists (e.g., cardiac rehabilitation, pulmonary rehabilitation). The patient may be seen for more than an hour a day, progressing in multiple intervention programs, including exercise, bronchopulmonary hygiene, and education concerning cardiovascular fitness.
Billing Example
The following case is an example of when the 93015 CPT code can be billed:
A 38-year-old male presents to ED with a chief complaint of dizziness. The patient reports vertigo began one day ago. Vertigo began while at home when he stood up.
The patient describes the course of vertigo as abrupt, and The dizziness is currently 6/10. Vertigo is worsened by standing, head movement, and movement. The vertigo is not worsened by breathing or lying supine.
The patient denies headache, back pain, abdominal pain, nausea, vomiting, diarrhea, changes in vision, urinary complaints, or other symptoms.
Anti-vertigo meds alleviate vertigo. Vertigo is associated with nausea, vomiting, and gait instability. Vertigo is not associated with a vision change.
The patient is morbidly obese and has a higher risk of heart disease. The physician-physician ordered multiple diagnostic tests: ECG, CMP, CBC, CT, MRI, and X-ray of the head and spine.
Diagnostic studies show that the patient had an irregular heartbeat and suggested Cardiac perfusion with the stress test, billed with CPT code 93015.


