99233 CPT Code (2022) – Description, Guidelines, Reimbursement, Modifiers & Examples
The 99233 CPT code is used to report services when subsequent or follow-up visits are rendered to the patient on the 2nd day of hospital admission by qualified healthcare professional or supervising physician or skilled clinician.
99233 CPT Code | Description
99233 CPT code does not differentiate between established and new patient visits.
A new patient is a patient who did not receive any professional services from a physician or other qualified healthcare professional with the same group or specialty within the past three years, while an established patient who did receive assistance in the past three years respectively by the same physician or same group or specialty.
Two other CPT codes are available for Subsequent hospital visits, which are 99231 and 99232.
These CPT codes typically require 15 and 25 minutes of total time spent by the physician during the encounter, while CPT 99233 requires at least 35 minutes of total time spent by the provider if codes selection is based on time.
CPT 92333 is considered the highest category amongst the other two CPT codes, 99231 and 99232, which are regarded as the lowest and moderate categories, respectively.
CPT 99233 required detailed history and exam and a high MDM level. In addition, 99233 CPT code includes the following service when it is billed:
- It typically requires 35 minutes beside the patient or on the hospital unit or floor.
- It includes reviewing medical records, diagnostic studies results, and any changes made in the patient’s treatment due to physical status or medical records after every prior assessment.
CPT 99233 is used to report services when rendered on the 2nd day of the hospital by the physician or other qualified healthcare professional at the bedside and the patient’s hospital floor or unit when code selection is time-based which requires at least two out three critical components of evaluation and management (E/M) codes. This CPT 99233 includes:
- Detailed physical exam
- Detailed history
- High level of medical decision making (MDM)
- The nature of presenting problem must reflect the patient’s current condition and Family needs.
- The patient presents with an unstable condition or significant new problem or complication.
- It typically requires 35 of total time spent by the provider at the bedside and on the patient’s hospital floor or unit when code selection is time-based
Reimbursement
The cost and RUVS of 99233 CPT code are as follows:
- Facility: Cost 109.55$ RUVS 3.16548
- Non-Facility: Cost 109.55$ RUVS 3.16548
Nowadays, telehealth services are frequently provided to patients due to COVID 19 situation. In this case, it is appropriate to attach modifier 95 with CPT 99233. Furthermore, if telehealth service is provided at the hospital due to some emergency, then it is reasonable to bill Q3014 for reporting telehealth services provided at the hospital.
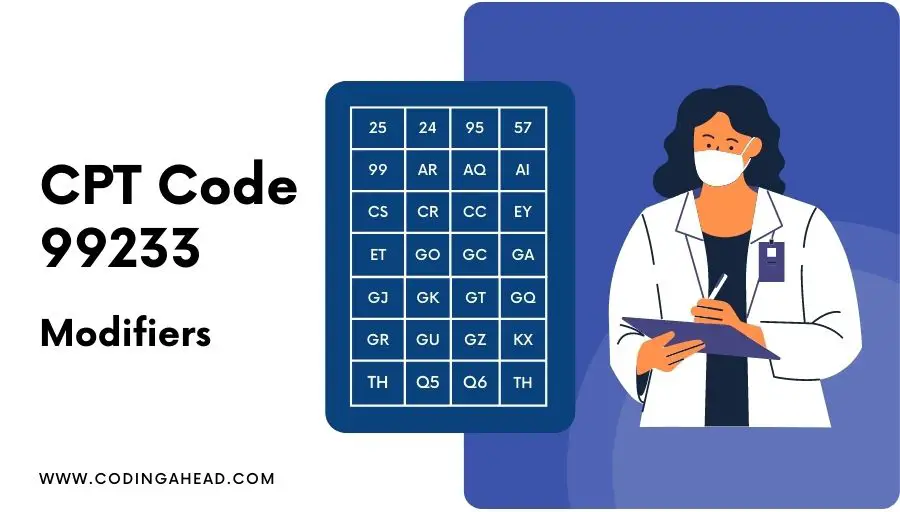
99233 CPT Code Modifiers
Modifier 25 will be appended with CPT 99233 when services are done in conjunction with other services generally not billed together on the same day. While 24 will be appended with services done in the postoperative period with unrelated procedures or services.
Modifier 95 will be attached to CPT 99233 if service is provided as a telehealth visit.
Modifier 57 will be attached to CPT 99233 if physicians plan to do surgery on the same service date when the E/M visit is done.
Billing & Coding Guidelines
99233 CPT code requires 2 out of 3 key components (history, exam, and medical decision making) to meet the criteria or exceed the level of service, which are as follows:
- Detailed history: It requires at least 4 HPI elements, 10 ROS systems, and one history component are needed 2 out of 3 components (PFSH).
- Detailed Exam: It requires eight-plus systems as per 95 documentation and a nine-plus system with two-plus bullets required per 97 documentations.
- High MDM: It requires at least two out three components of MDM that must be met on that basis of risk, diagnostic or treatment, Data management services like Medicine, Laboratory, Medicine, Medicine, Medicine, Medicine, review, counseling, Interpretation of services.
If time is mentioned in the medical notes, it is appropriate to bill based on time instead of MDM, which typically requires 35 minutes on the patient’s hospital floor or unit.
If E/M selection is time-based of CPT 99233, then coordination of care or counseling must reach the half time of the physician spent on the hospital floor or unit for patient care.
Both documentations guidelines 1995 and 19997 are acceptable for CPT 99233.
It includes all the reviewing of diagnostic studies results, medical records, and changes in the treatment since the last examination was done.
CPT 92333 will be reported for subsequent or follow-up services only. There are different CPT codes for Initial hospital visits (CPT 99221-99223). CPT (99238-99239) will be reported if a patient is discharged on different service dates. On the other hand, if the patient’s discharge is on the same date of admission, CPT (99234-99236) will be notified.
Documentation should support the medical necessity of the service, and it is medically appropriate.
Emergency CPT codes (99281-99285) are not allowed to bill together with CPT 99233, and the modifier is also not applicable.
99233 CPT code includes all the services reported on admission date in other settings or departments associated with observation status admission will be reported separately with these CPT (99202-99215, 99281-99285, 99304-99318, 99324-99337, 99341-99350, 99381-99397).
Q3014 is applicable when the hospital provides telemedicine service as an origin site to other outpatient hospital patients.
If inpatient service is provided by another physician instead of admitting physician, any subsequent visit would be reported separately with CPT 99232.
Examples
Below are examples of when it is appropriate to use CPT 99233 code.
Example 1
Two days ago, a 52-year-old female was admitted to the hospital presenting with generalized weakness, vomiting x1, and dysuria x1 days. The patient has a follow-up visit today as medication and treatment are not getting better. The patient reports a chill today with left flank pain and suprapubic pain.
She has some mild lightheadedness but denies chest pain, palpitations, syncope, diarrhea, hematuria. The physician ordered to repeat all the radiology and pathology tests to confirm the patient’s current condition.
The physician had consulted with a gastroenterologist, and he had advised for the EGD procedure. The physician made an appointment for an EGD procedure by tomorrow.
Example 2
A 46-year-old male with a past medical history of moderate intellectual disability, cerebral palsy, type 2 Diabetes Mellitus, BPH is here for a follow-up visit of hyperglycemia and increased urinary frequency today and was admitted to the hospital five days ago. Labs and pathology test shows that the patient’s sugar level is still high at 450 and not stabilized yet.
The physician prescribed some new medication and treatments. He also ordered multiple tests from the radiology, medicine, laboratory, and pathology sections.
The patient has an immediate threat to life and chances of organ failure if the patient’s condition does not become stable in the next 2 to three hours.
The physician had consulted with an endocrinologist for hyperglycemia and management options. Patient conditions are getting better after the medication change, and sugar levels drop to 300.
Example 3
60-year-old male denies PMHX presents c/o constant midsternal chest pain two days ago, intermittent chest pain, and admitted to the hospital. Today, the patient has a pressure-like sensation with intermittent shortness of breath.
The patient denies any pain at this time. The patient reports severe chest pain two weeks ago at 1-hour intervals.
He denies trauma, heavy lifting, palpitations, dizziness, cough, recent illness, fever, chills, back pain, abdominal pain, nausea, recent travel, known sick contacts, current antibiotic use, near-syncope, or syncope, changes in stool color, urinary complaints, or any other symptoms.
The patient did not take any medication for pain. The patient vapes and drinks alcohol on occasion but denies illicit drug use. The physician ordered an EKG, CT and MRI, and an X-ray of the chest.
The studies showed abnormal EKG and Acute coronary syndrome. The physician consulted with the Cardiologist for further treatment.
Example 4
A 62-year-old female is presented to the emergency department. She has a past medical history of type 2 diabetes, essential hypertension, IBS, multiple episodes of constipation in the past requiring ileostomy.
She complained of lower abdominal pain and constipation and was admitted to the hospital yesterday. The patient’s condition progressively got worse yesterday at the emergency room ER. The physician attempted a manual disc impaction.
However, the CAT scan of the abdomen after the procedure showed the patient was still constipated and was in pain.
She also complained of associated rectal bleeding. The patient denies using opiate medication at home and denies chest pain, shortness of breath, fever, chills, nausea, vomiting, urinary symptoms.
The physicians had ordered to repeat all the labs, radiology, and medical section tests to determine the patient’s current condition and make some medication changes.
The patient may need an immediate endoscopic procedure and had consulted with a specialist for further treatment and management options.
More Examples
Example 1
Subsequent hospital visit for a 38-year-old male, quadriplegic with acute autonomic hyperreflexia, who is not responsive to initial care. (Physical Medicine & Rehabilitation)
Example 2
Follow-up hospital visit for a teenage female who continues to experience severely disruptive, violent, and life-threatening symptoms in a complicated multi-system illness, Family/social circumstances also a contributing factor. (Psychiatry)
Example 3
Subsequent hospital visit for a 42-year-old female with progressive systemic sclerosis (scleroderma), renal failure on dialysis, congestive heart failure, cardiac arrhythmias, and digital ulcer. (Allergy & Immunology)
Example 4
Subsequent hospital visit for a 50-year-old diabetic, hypertensive male with non responding back pain and radiating pain to the lower left extremity, who develops chest pain, cough, and bloody sputum. (Orthopaedic Surgery)
Example 5
Subsequent hospital visit for a 64-year-old female, status post-abdominal aortic aneurysm resection, with non-responsive coagulopathy, who has now developed lower Gl bleeding. (Abdominal Surgery/Colon & Rectal Surgery/General Surgery)
Example 6
Follow-up hospital care of patient with pansinusitis infection complicated by a brain abscess and asthma; no response to current treatment. (Otolaryngology/Head & Neck Surgery)
Example 7
Subsequent hospital visit for a patient with a laryngeal neoplasm who develops airway compromise, suspected metastasis. (Otolaryngology/Head & Neck Surgery)
Example 8
Subsequent hospital visit for a 49-year-old male with significant rectal bleeding, etiology undetermined, not responding to treatment. (Abdominal Surgery/General Surgery/Colon & Rectal Surgery)
Example 9
Subsequent hospital visit for a 50-year-old male, post-aortocoronary bypass surgery; now develops hypotension and oliguria. (Cardiology)
Example 10
Subsequent hospital visit for an adolescent patient who is violent, unsafe, and noncompliant, who multiple expectations for participation in treatment plan and behaviour on the treatment unit. (Psychiatry)
Example 11
Subsequent hospital visit for an 18-year-old male being treatment for presumed PCP psychosis, Patient is still moderately symptomatic with auditory hallucinations and is insisting on signing out against medical advice. (Psychiatry)
Example 12
Subsequent hospital visit for an 8-year-old female with caustic ingestion now has fever, dyspnea, and dropping hemoglobin. (Gastroenterology)
Example 13
Follow-up hospital visit for a chronic renal failure patient on dialysis who develops chest pain, shortness of breath, and a new onset pericardial friction rub. (Nephrology)
Example 14
Subsequent hospital visit for a 44-year-old patient with electrical burns the left arm with ascending infection. (Orthopaedic Surgery)
Example 15
Subsequent hospital visit for a patient with systemic sclerosis aspirated and short of breath. (Dermatology)
Example 16
Subsequent hospital visit for a 65-year-old female, status postoperative resection of abdominal aortic aneurysm, with suspected ischemic bowel. (General Surgery)
Example 17
Subsequent hospital visit for a 50-year-old male, post-aortocoronary bypass Surgery, now develops hypotension and oliguria. (Cardiology)
Example 18
Subsequent hospital visit for a 50-year-old male, following an acute myocardial infarction, who complains of shortness of breath and new chest pain. (Cardiology)
Example 19
Subsequent hospital visit for a 65-year-old female with rheumatoid arthritis (stage 3, class 3) admitted for urosepsis, On the third hospital day, chest pain, dyspnea, and fever develop. (Rheumatology)
Example 20
Follow-up hospital care of pediatric case with stridor, laryngomalacia, established tracheostomy, complicated by multiple medical problems in PICU. (Otolarygology/Head & Neck Surgery)
Example 21
Subsequent hospital visit for a 60-year-old female, four days post uncomplicated inferior myocardial infraction who has developed severe chest pain, dyspnea, diaphoresis, and nausea. (Family Medicine)
Example 22
Subsequent hospital visit for a patient with AMLL (acute myelogenous leukemia), fever, elevated white count and uric acid undergoing induction chemotherapy. (Hematology/Oncology)
Example 23
Subsequent hospital visit for a 38-year-old quadriplegic male with acute autonomic hyperreflexia, who is not responsive to initial care. (Physical Medicine & Rehabilitation)
Example 24
Subsequent hospital visit for a 65-year-old female postoperative resection of abdominal aortic aneurysm, with suspected ischemic bowel. (General Surgery)
Example 25
Subsequent hospital visit for a 60-year-old female with persistent leukocytosis and a fever seven day after a sigmoid colon resection for carcinoma. (Infectious Disease)
Example 26
Subsequent hospital visit for a chronic renal failure patient on dialysis, who develops chest pain, shortness of breath, and new onset pericardial friction rub. (Nephrology)
Example 27
Subsequent hospital visit for a 65-year-old male with acute myocardial infraction who now demonstrates complete heart block and congestive heart failure. (Cardiology)
Example 28
Subsequent hospital visit for a 25-year-old female with hypertension an systemic lupus erythematosus, admitted for fever and respiratory distress, On the third hospital day, the patient presented with purpuric skin lesions and acute renal failure. (Allergy & Immunology)
Example 29
Subsequent hospital visit for a 55-year-old male with severe chronic obstructive pulmonary disease and bronchospasm; initially admitted for acute respiratory distress requiring ventilator support in the ICU. The patient was stabilized, extubated, and transferred to the floor but has now developed acute fever, dyspnea, left lower lobe rhonchi, and laboratory evidence of carbon dioxide retention and hypoxemia. (Family Medicine/Internal Medicine)
Example 30
Subsequent hospital visit for 46-year-old female, known liver cirrhosis patient, with recent upper gastrointestinal hemorrhage from varices; now with worsening ascites and encephalopathy. (Gastroenterology)
Example 31
Subsequent hospital visit for 62-year-old female admitted with acute subarachnoid hemorrhage, hegative cerebral arteriogram, increased lethargy, and hemiparesis with fever. (Neurosurgery)



