Acupuncture CPT Codes (2022) Description, Guidelines, Reimbursement, Modifiers & Example
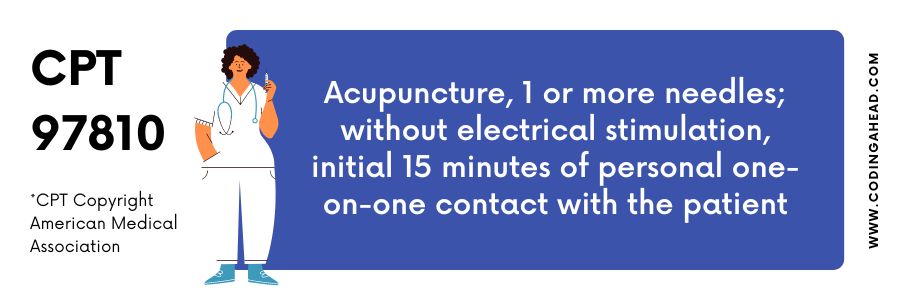
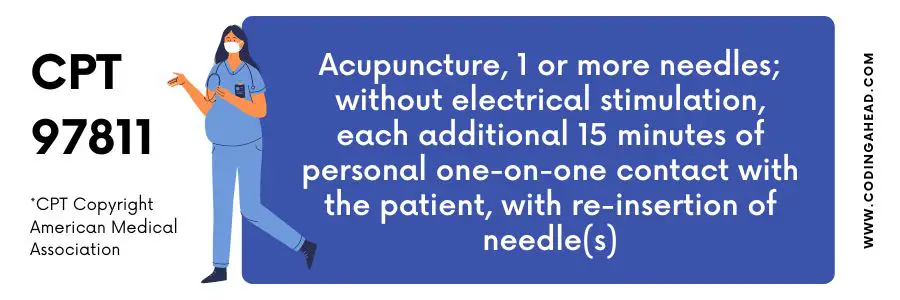
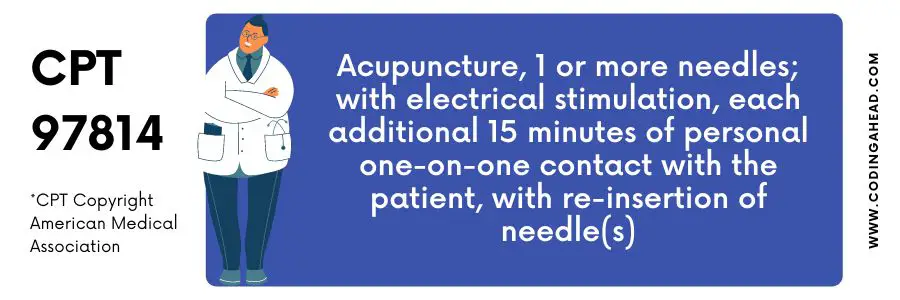
Acupuncture CPT codes 97810 – 97814 are part of the American Medical Association’s Current Procedural Terminology (CPT) code set for medical services and procedures. Four codes cover most acupuncture services to bill insurance for acupuncture services. Electrical stimulation will require updating the CPT codes for acupuncture.
Summary
15-minute needle insertion time and one-on-one time with the patient are required for Acupuncture CPT code 97810. After the initial 15 minutes, use one unit for every 15 minutes of personal one-on-one contact with the patient, including re-insertion of needles, according to CTP code 97811.
CTP code 97813 specifies a 15-minute needle insertion and one-on-one contact with the patient. According to CTP code 97814, one unit may use for every 15 minutes of additional one-on-one contact with the patient, including re-insertion of needles.
On January 21st, 2020, the CMS announced that Medicare and Medicaid now cover chronic low back pain. This term refers to localized lower back discomfort that has lasted more than three months. Despite this ruling, there are still several conditions that must be met for Medicare to fund acupuncture services.
Medicare guidelines currently cover the following acupuncture billing codes (at the current Medicare national average fee schedule). This page may use to seek up local area codes depending on where you live—acupuncture at the start (97810).
TIP: You can find the complete billing guide for CPT code 97810 here.
Inserting the first needle takes about 15 minutes with one-on-one contact with the patient. This report cannot utilize either Acupuncture CPT codes 97813 or 97812.
Intraservice treatment times include hand cleansing, site selection, cleaning, insertion/stimulation/removal/property disposal. Therapists undertake treatment efficacy evaluations, engage with patients and families (including education, discussion, and counseling), and prepare for future therapy sessions.
These methods demonstrate that daily evaluation is a vital component of acupuncture treatment. A re-examination takes about 30 days to complete. A 30-day re-evaluation of acupuncture may require traditional procedures and the usual day-to-day assessment, for example, if the patient receives a new diagnosis or if the patient’s condition suddenly changes.
When a patient’s distinct possibility necessitates additional E&M services beyond the typical pre- and post-acupuncture evaluation and management work, consideration may give to categorizing E&M services. Situations like this are all too common.
Acupuncture CPT Codes Description
Acupuncture is a covered benefit for groups who have purchased the acupuncture rider or have an acupuncture benefit. Subscriber agreements, benefit booklets, and proof of coverage all have information about acupuncture benefits.
An acupuncturist inserts needles into the skin at specific points on the body to produce anesthesia, alleviate pain, treat various non-painful ailments, and alleviate opiate withdrawal symptoms.
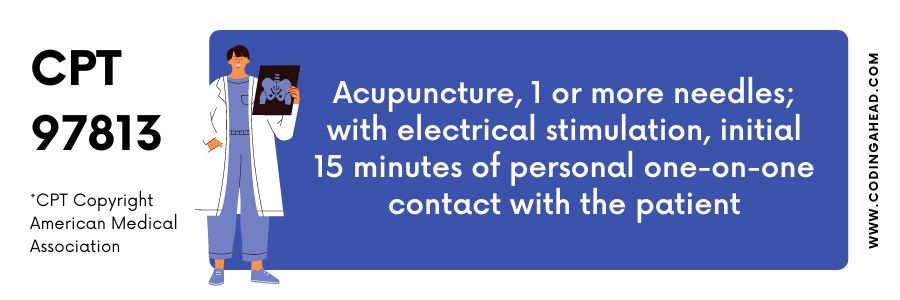
Initial Acupuncture with Electrical Stimulation (97813) For the initial patient evaluation, office visits, also known as assessment and management services, may be charged. Every 30 days or every six visits is a decent rule of thumb.
Because each day’s therapy includes evaluation and management, billing these CPT codes each time a patient receives acupuncture is ineffective. There are four CPT codes for this in acupuncture.
When you initially see a patient, use Acupuncture CPT codes 99201 through 99204 to bill a new patient visit code. A “new patient” is someone who joins your practice after having not seen you or another specialist in the same specialty in the preceding three years.
Acupuncture CPT Codes Billing Guidelines
Holistic practices have an additional layer of complexity in insurance billing. CPT codes may use to document the vast majority of medical procedures performed by healthcare professionals. Doctors may bill insurance companies appropriately and get reimbursed for their services using these medical billing codes.
It is common for acupuncture clinics to use unique identifiers for their services. Acupuncture CPT codes will differ in duration because treatments may often tag in 15-minute intervals, so one code will use for the first 15 minutes of service and another for the next 15 minutes.
The vast majority of medical operations performed by health care practitioners may document using CPT codes. Doctors can bill insurance companies and receive reimbursement for their services using these medical billing codes.
Acupuncture clinics frequently employ unique identities for their services. Because services may often code in 15-minute increments, you’ll need one code for the first 15 minutes of service and a unique code for each succeeding unit of time. To update your acupuncture CPT codes, you must use electrical stimulation.
CPT codes for acupuncture sessions, office visits, and physical therapy-based treatments and modalities may organize by your practice’s three primary revenue sources. Remember that the plan and the employer determine your patient’s insurance coverage; simply knowing the insurance company’s name is insufficient.
When billing insurance for acupuncture, always confirm your patient’s benefits with the payer before initiating treatment. Specific Medicare requirements apply to acupuncture as well.
Your practice will use one code for the first 15 minutes and a separate code for each subsequent visit to bill acupuncture treatments. You can only amend your acupuncture billing codes if you employ electrical stimulation.
After the initial 15 minutes of one-on-one interaction, continue to use one unit for every 15 minutes of personal connection and needle re-insertion with the patient. This item produces the same outcomes as 97810 when coupled with 97813.
Acupuncture CPT Codes Modifiers
Pre, intra-, and post-service assessments associated with the E&M acupuncture codes may utilize in addition to the evaluations linked to the E&M acupuncture codes. E&M codes with acupuncture can be invoiced using modifier -25 to indicate this difference in treatment. Without this change, the E&M service will instantly cancel.
E&M and acupuncture services will not be affected by utilizing this modification. As acupuncturists make the most common coding and billing error, many in the field incorrectly feel that they cannot be paid for an exam as they never billed it appropriately.
An E&M treatment, including acupuncture, has never been paid for before, which should ease your initial trepidation. You merely didn’t have the correct code and modifiers in your system.
You can find the direct instructions on pages 658-659 in CPT 2016. “Physician or other health care professional evaluation and management (E&M) services may be billed separately utilizing modifier -25 for patients who require significant, individually identifiable E&M services in addition to pre-and post-acupuncture therapy.
It is not included in the acupuncture service how much time will spend on the E/M service. Acupuncture is an appropriate treatment technique for various ailments, but you must first examine your patient to see if acupuncture is right.
It may consider unprofessional if an examination may not perform before the start of treatment. Modifier -25 may append to the code to show E&M as a distinct reimbursable service on the invoice.
Even though they may acknowledge it may examine, routine follow-up appointments may not regard in addition to the acupuncture codes and services may evaluate. Understanding the acupuncture codes and benefits is essential to this protocol’s comprehension. Pre-, intra-, and post-service evaluations may include the acupuncture service.
The Acupuncture CPT codes 97810 through 97814 incorporate evaluation and management as part of the total daily therapy. Charging these codes for every single patient who receives acupuncture is not appropriate.
Before seeing a patient in person, a physician should thoroughly review the patient’s file, an interim history, and any necessary physical examination and assessment. Treatment times that include hand washing, site selection, cleanliness, insertion/stimulation/removal/proper disposal are known as interservice.
As part of post-service activities, therapists conduct evaluations of treatment effectiveness, communicate with patients and families (including education, discussion, and counseling), and plan for future therapy sessions.
These protocols make it apparent that daily evaluation is essential for acupuncture treatment. In addition to the routine day-to-day assessment, a re-examination takes roughly 30 days to complete according to traditional methods.
Consideration may give to categorizing E&M services in cases where a patient’s unique circumstance needs additional E&M services beyond the standard pre- and post-acupuncture evaluation and management work.
For instance, if the patient receives a new diagnosis or whose condition changes drastically, a 30-day re-evaluation of acupuncture may be necessary. Situations like these are commonplace.
In addition to the evaluations associated with the E&M acupuncture codes, pre-, intra-, and post-service assessments related to the E&M acupuncture codes may use. The E&M evaluation as part of the acupuncture services differs from and supplements the acupuncture evaluation signified by the -25 modification.
Without this modification, the E&M service will terminate immediately. This adjustment will not affect E&M or acupuncture services. Many acupuncturists wrongly believe that they cannot be paid for an exam because they never invoiced it properly, which is the most common coding and billing error committed by practitioners.
An E&M therapy that includes acupuncture has never been paid for previously, which should alleviate your initial concerns. You just lacked the necessary code and modifiers in your system.
It may regard as unprofessional not to evaluate the start of treatment. Modifier -25 may add to the code for E&M to appear as a separately reimbursable service on the invoice.
The modifiers for Acupuncture CPT Codes are 25.
Acupuncture CPT Codes Reimbursement
Based on current relative value units and the $36.086 Medicare conversion factor for 2020, the primary code 97810 (the first 15 minutes) in the office setting will reimburse $38. The cost of each 15-minute increment of the add-on code 97811 should be $28. (All fees are the same no matter where you live.)
To get efficient remuneration for services, every medical practice, whether traditional or holistic, must follow proper billing practices. Accurate billing codes benefit insurance companies and patients by providing a legal record of their treatment.
Example
An established patient has received professional services from you or another provider in the same specialty for at least three years and is a member of your practice. Billing an established patient visit (Acupuncture CPT codes 97810-97814) on each visit is improper because regular acupuncture treatment codes already include a daily evaluation component to measure your patient’s development.



