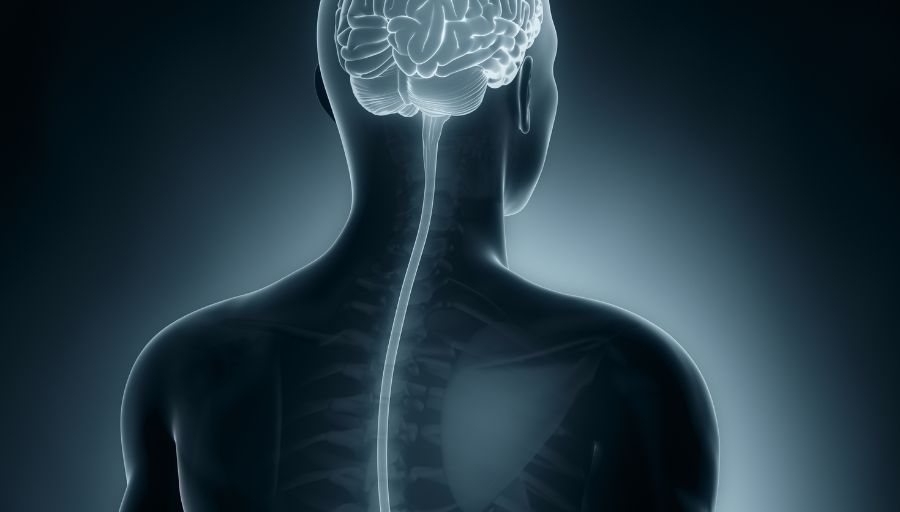
Tuberculosis Unmasked: Brain and Spinal Cord Tuberculomas, Meningoencephalitis, Neuritis, and Polyneuropathy
This article discusses Tuberculoma of the brain and spinal cord, Tuberculous meningoencephalitis, Tuberculous neuritis, and Tuberculous polyneuropathy.
1. Tuberculoma of the brain and spinal cord
Tuberculoma of the brain and spinal cord refers to firm, avascular, spherical masses in the brain and spinal cord (a group of nerve fibers encased in the vertebral column connecting the brain to the rest of the body), a manifestation of tuberculosis (TB) caused by Mycobacterium tuberculosis, which can occur even under appropriate antitubercular therapy.
Tuberculoma of the brain and spinal cord is also referred to as a Tuberculous abscess of brain and spinal cord.
1.1 Symptoms
A patient with tuberculoma of the brain and spinal cord can experience;
- fever;
- headache;
- stiff neck with focal neurological deficits;
- behavioral changes, and
- an altered mental status.
Children might experience seizures and abdominal symptoms such as nausea and vomiting.
1.2 Diagnosis
Providers diagnose the condition based on positive reports of the patient’s cerebrospinal fluid (CSF) for M. tuberculosis, tuberculin skin test, and previous history of tuberculosis or active disease. MRI or CT scans reveal the presence of tuberculoma(s).
1.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. Surgical therapy may be employed to remove the tuberculoma(s).
2. Tuberculous meningoencephalitis
Tuberculous meningoencephalitis is a manifestation of tuberculosis (TB) of the central nervous system due to infection by Mycobacterium tuberculosis that causes inflammation or swelling of the meninges (membranes around the brain and spinal cord) and the brain, which can occur even under appropriate antitubercular therapy.
Tuberculous meningoencephalitis is also referred to as Tuberculous myelitis.
2.1 Symptoms
A patient with tuberculous meningoencephalitis experiences;
- fever;
- paresis (weakness);
- anorexia (loss of appetite);
- myalgia (muscle aches);
- headache;
- stiff neck along with focal neurological deficits;
- behavioral changes;
- altered mental status.
Children might experience night sweats, seizures, and abdominal symptoms such as nausea and vomiting.
2.2 Diagnosis
Providers diagnose the condition based on positive reports of the patient’s cerebrospinal fluid (CSF) for M. tuberculosis, tuberculin skin test, and previous history of tuberculosis or active disease. MRI or CT is also indicated.
2.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. In severe cases, surgical therapy is indicated to treat hydrocephalus, tuberculous tumors (tuberculomas), and abscesses. There is a high mortality rate for this condition.
3. Tuberculous neuritis
Tuberculous neuritis, also referred to as tuberculous mononeuropathy, is a manifestation of tuberculosis (TB) of the nervous system due to Mycobacterium tuberculosis that causes inflammation of a single nerve or nerve group, which can occur even under appropriate antitubercular therapy.
3.1 Symptoms
A patient with tuberculous neuritis may experience;
- local pain with swelling at the site of the affected nerve;
- paresthesia (pins and needle sensation);
- paresis (weakness);
- numbness along with focal neurological deficits;
- behavioral changes, and
- altered mental status.
3.2 Diagnosis
Providers diagnose the condition based on positive reports of the patient’s cerebrospinal fluid (CSF) for M. tuberculosis, tuberculin skin test, and previous history of tuberculosis or active disease. MRI or CT may be indicated.
3.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. In severe cases, surgical therapy is indicated to treat tuberculous tumors (tuberculomas or granulomas) and abscesses.
4. Tuberculous polyneuropathy
Tuberculous polyneuropathy (damage to more than one nerve or nerve group) is a rare but highly devastating manifestation of tuberculosis (TB) caused by Mycobacterium tuberculosis, which can occur even under appropriate antitubercular therapy.
4.1 Symptoms
A patient with Tuberculous polyneuropathy experiences;
- paresthesia;
- hypoesthesia (reduced touch and sensation);
- fever;
- headache;
- focal neurological deficits;
- behavioral changes;
- paresis (weakness);
- numbness;
- altered mental status.
4.2 Diagnosis
Providers diagnose the condition based on positive reports of specimens for M. tuberculosis, tuberculin skin test, and previous history of tuberculosis or active disease. MRI or CT may be indicated.
4.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. In severe cases, surgical therapy is indicated to remove tuberculous tumors (tuberculomas or granulomas).