Tuberculosis | Four Types Explained
Below, we describe four types of Tuberculosis. Firstly, we’ll explain Respiratory Tuberculosis, then Tuberculosis of the nervous system, followed by Tuberculosis of other organs, and lastly, Miliary Tuberculosis.
1. Respiratory Tuberculosis
The bacterium Mycobacterium tuberculosis (M. tuberculosis), typically spread by airborne infection, person–to–person contact or cough or sneeze of an infected person, causes respiratory or pulmonary Tuberculosis (TB).
Most patients who develop TB were exposed or had repeated exposure months or years prior, but some patients, notably babies and children, can develop primary TB from the initial exposure.
1.1 Symptoms
A patient with Respiratory Tuberculosis can experience:
- severe difficulty breathing;
- cough with mucus or blood;
- chest pain, wheezing;
- fatigue, weight loss;
- fever; and
- excessive night sweats.
1.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination.
The provider may perform tests such as bronchoscopy, chest X–ray or CT scan, and tuberculin skin test. Laboratory tests of the patient’s sputum can detect the organism.
1.3 Treatment
Treatment commonly includes taking a combination of 4 medicines: isoniazid, rifampin, ethambutol, and pyrazinamide for six months or longer.
The most commonly followed approach is the DOT, or directly observed therapy, to ensure proper course completion.
2. Tuberculosis of the nervous system
Tuberculosis of the nervous system is a rare but highly devastating manifestation of Tuberculosis (TB) caused by Mycobacterium tuberculosis that affects the brain, spinal cord, and meninges (membranes covering the spinal cord and brain), which can occur even under appropriate antitubercular therapy.
2.1 Symptoms
A patient with central nervous system (CNS) tuberculosis experiences;
- fever;
- headache;
- stiff neck;
- focal neurological deficits;
- behavioral changes, and
- an altered mental status.
Children might experience seizures and abdominal symptoms such as nausea and vomiting.
2.2 Diagnosis
Providers diagnose the condition based on positive reports of the patient’s cerebrospinal fluid for Mycobacterium tuberculosis, tuberculin skin test, and previous history of Tuberculosis or active disease. MRI or CT is also indicated.
2.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. In severe cases, surgical therapy is indicated to treat hydrocephalus, tuberculous tumors (tuberculomas), and brain abscesses.
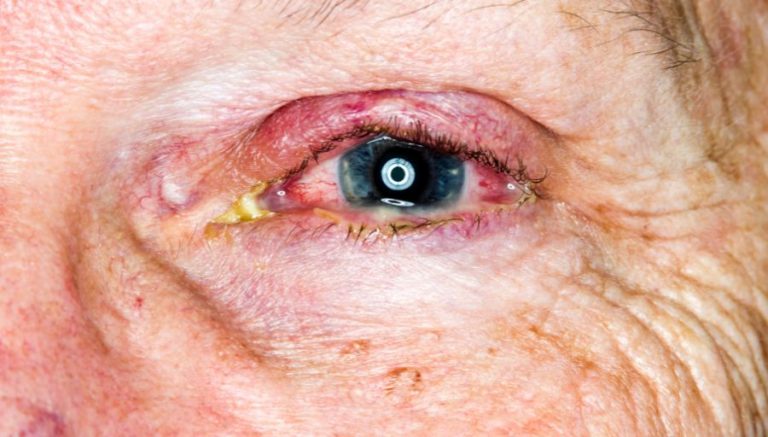
3. Tuberculosis of other organs
Tuberculosis (TB) of other organs is caused by Mycobacterium tuberculosis, which enters through the respiratory system; the bacilli (rod–shaped bacterium) migrate to other organ systems through the lymph system or blood circulation and forms granulomas (inflammatory masses of cells), which can remain dormant for long periods but eventually rupture and infect the involved organ.
3.1 Symptoms
A patient with TB of other organ systems experiences various symptoms depending on the organ system involved.
The formation of granulomas or tuberculomas (tuberculous” tumors”) can result in fibrosis (thickened and scarred connective tissue), leading to obstruction due to stricture or stenosis (narrowing of a tubular structure).
The patient may experience other typical symptoms of TB, such as night sweats, fever, weight loss, and pain and inflammation in the organ system affected.
3.2 Diagnosis
Providers diagnose the condition based on blood tests, tuberculin skin tests, and previous Tuberculosis or active disease history. MRI or CT may detect granulomas or tuberculomas.
3.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9–12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation.
The provider may perform surgery to treat abscesses, tuberculomas, and strictures or obstructions.
4. Miliary Tuberculosis
Miliary Tuberculosis is a rare but highly devastating manifestation of Tuberculosis (TB) that can occur even under appropriate antitubercular therapy; it is caused by Mycobacterium tuberculosis that enters the bloodstream and affects multiple sites of the body, such as the brain, liver, and spleen, or kidney. Millet seed–like changes appear on the chest X–ray.
4.1 Symptoms
A patient with military Tuberculosis experiences:
- fever;
- headache;
- weight loss;
- blood in the sputum;
- chest pain;
- stiff neck;
- focal neurological deficits;
- behavioral changes;
- altered mental status;
- liver and spleen enlargement;
- adrenal insufficiency; and
- lymphadenopathy.
Children might experience seizures and gastrointestinal symptoms such as nausea and vomiting.
4.2 Diagnosis
Providers diagnose the condition based on positive reports of the patient’s cerebrospinal fluid for Mycobacterium tuberculosis, tuberculin skin test, and previous history of Tuberculosis or active disease. X–ray, MRI, or CT is also indicated.
4.3 Treatment
Treatment includes standard antituberculous chemotherapy, starting with isoniazid, rifampin, rifabutin, pyrazinamide, and ethambutol for two months, followed by longer-term (9 to 12 months) isoniazid, rifabutin, and rifampin for maintenance; other drugs may be tried if these drugs are ineffective.
At times, adjunctive steroid therapy helps treat symptoms of swelling and inflammation. In severe cases, surgical therapy is indicated to treat liver and brain abscesses, hydrocephalus, or tuberculous tumors (tuberculomas).