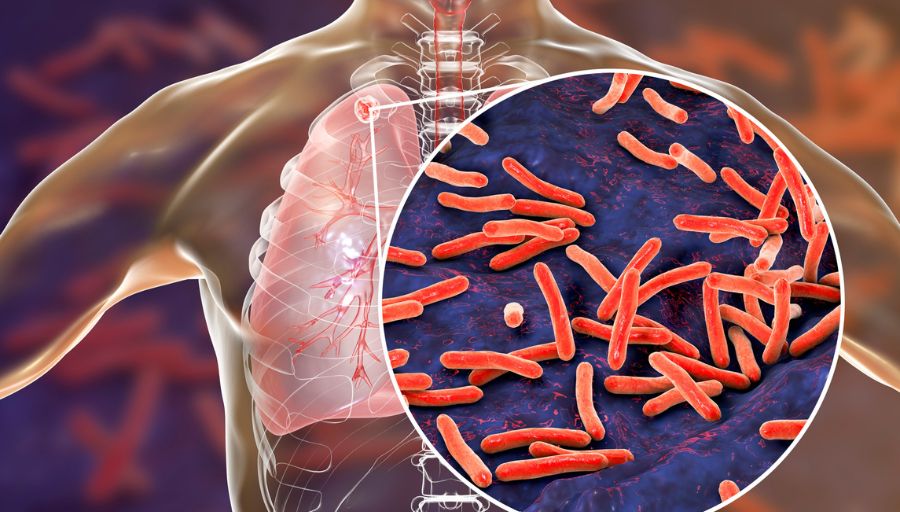
A Detailed Examination of Respiratory Tuberculosis: Types, Symptoms, Diagnosis, and Treatment
There are five types of Respiratory Tuberculosis. Namely, Tuberculosis of the lung, Tuberculosis of intrathoracic lymph nodes, Tuberculosis of the larynx, trachea, and bronchus, Tuberculous pleurisy, and the last type is Primary respiratory Tuberculosis.
1. Tuberculosis of the lung
The bacterium Mycobacterium tuberculosis (M. tuberculosis), typically spread by airborne infection, person–to–person contact, or cough or sneeze of an infected person, causes Tuberculosis (TB) of the lung.
Most patients who develop TB were exposed or had repeated exposure months or years prior, but some patients, notably babies and children, can develop primary TB from the initial exposure.
Tuberculosis of the lung is also referred to as:
- Tuberculous bronchiectasis
- Tuberculous fibrosis of the lung
- Tuberculous pneumonia
- Tuberculous pneumothorax
1.1 Symptoms
A patient with lung Tuberculosis can experience;
- severe difficulty breathing;
- cough with mucus or blood;
- chest pain;
- wheezing;
- fatigue;
- weight loss;
- fever; and
- excessive night sweats.
1.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination. The provider may perform tests such as bronchoscopy, chest X–ray or CT scan, and tuberculin skin test. Laboratory tests of the patient’s sputum can detect the organism.
1.3 Treatment
Treatment commonly includes taking a combination of 4 medicines, isoniazid, rifampin, ethambutol, and pyrazinamide, for six months or longer. The most commonly followed approach is the DOT, or directly observed therapy, to ensure proper course completion.
2. Tuberculosis of intrathoracic lymph nodes
The bacterium Mycobacterium tuberculosis (M. tuberculosis), typically spread by airborne infection, person–to–person contact, or cough or sneeze of an infected person, causes Tuberculosis (TB) of the intrathoracic lymph nodes.
This manifestation generally results from a primary infection in children, teenagers, and young adults. It can affect older adults as a secondary manifestation of an earlier TB infection.
Tuberculosis of intrathoracic lymph nodes is also referred to as:
- Tuberculosis of hilar lymph nodes
- Tuberculosis of mediastinal lymph nodes
- Tuberculosis of tracheobronchial lymph nodes
2.1 Symptoms
A patient with Tuberculosis of the intrathoracic lymph nodes can experience;
- fever;
- loss of appetite;
- difficulty breathing;
- fatigue;
- weight loss;
- excessive night sweats; and
- an overall deterioration of health.
2.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination. The provider may perform tests such as bronchoscopy, chest X–ray or CT scan, and tuberculin skin test. Laboratory tests of the patient’s sputum can detect the organism.
2.3 Treatment
Treatment commonly includes taking a combination of 4 medicines: isoniazid, rifampin, ethambutol, and pyrazinamide for six months or longer. The most commonly followed approach is the DOT or directly observed therapy, which ensures proper course completion. Providers may perform surgery to remove the infected lymph nodes.
3. Tuberculosis of the larynx, trachea, and bronchus
The bacterium Mycobacterium tuberculosis (M. tuberculosis), typically spread by airborne infection, person–to–person contact, or cough or sneeze of an infected person, causes Tuberculosis (TB) of the larynx, trachea, and bronchus. This infection affects the upper respiratory system.
Tuberculosis of the larynx, trachea, and bronchus covers;
- Tuberculosis of bronchus
- Tuberculosis of glottis
- Tuberculosis of larynx
- Tuberculosis of trachea
3.1 Symptoms
A patient with Tuberculosis of the larynx, trachea, and bronchus can experience;
- loss of appetite;
- difficulty in breathing;
- hoarseness of voice;
- cough with mucus or blood;
- sore throat;
- fatigue;
- weight loss;
- excessive night sweats;
- mild fever; and an
- the overall deterioration of health.
3.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination. The provider may perform tests such as bronchoscopy, chest X–ray, CT scan of the respiratory system, and tuberculin skin test. Laboratory tests of the patient’s sputum can detect the organism.
3.3 Treatment
Treatment commonly includes taking a combination of 4 medicines: isoniazid, rifampin, ethambutol, and pyrazinamide for six months or longer. The most commonly followed approach is the DOT, or directly observed therapy, to ensure proper course completion. In severe cases, the provider may perform tracheal resection.
4. Tuberculous pleurisy
Tuberculous pleurisy is an inflammation of the tissue lining the chest cavity and covering the lungs due to infection by the bacterium Mycobacterium tuberculosis (M. tuberculosis), which causes Tuberculosis (TB).
Tuberculous pleurisy is also known as Tuberculosis of pleura Tuberculous empyema.
4.1 Symptoms
A patient with tuberculous pleurisy can experience;
- pleuritic chest pain;
- nonproductive cough;
- breathing difficulty;
- fatigue;
- weight loss;
- excessive night sweats; and
- fever.
4.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination. The provider may perform tests such as chest X–ray and CT scan. Laboratory tests of the patient’s sputum, pleural fluid, or pleural biopsy can detect the organism.
4.3 Treatment
Treatment commonly includes chemotherapy, inflammatory drugs such as corticosteroids, and pleural fluid drainage, if required.
5. Primary respiratory Tuberculosis
The bacterium Mycobacterium tuberculosis (M. tuberculosis), typically spread by airborne infection, person–to–person contact, or cough or sneeze of an infected person, causes primary respiratory or pulmonary Tuberculosis (TB), an infection that commonly occurs in babies and children less than five years old who were not previously exposed to the bacteria.
5.1 Symptoms
A patient with primary respiratory Tuberculosis can experience;
- severe difficulty breathing;
- cough with mucus or blood;
- chest pain;
- wheezing;
- fatigue;
- weight loss;
- fever; and
- excessive night sweats.
5.2 Diagnosis
Providers diagnose the condition based on the patient’s symptoms, history, and physical examination. The provider may perform tests such as bronchoscopy, chest X–ray or CT scan, and tuberculin skin test. Laboratory tests of the patient’s sputum can detect the organism.
5.3 Treatment
Treatment commonly includes taking a combination of 4 medicines: isoniazid, rifampin, ethambutol, and pyrazinamide for six months or longer. The most commonly followed approach is the DOT, or directly observed therapy, to ensure proper course completion.