99213 CPT Code (2023) Description, Guidelines, Reimbursement, Modifiers & Examples
99213 CPT code billing is made easier with our coding guidelines, including a full description, modifiers, and reimbursement for CPT 99213. Office or other outpatient visit codes are typically reported daily and are differentiated as new or established patients. There are five levels under the services of office or other outpatient visits for the Established patient category represented by 99211-99215.
99213 CPT Code | Summary
These codes report office or other outpatient services for only established patients. 99213 CPT code is the low-level E&M code and includes straightforward medical decision-making.
According to medical coding and billing guidelines, An Established patientis the one who has received professional services from a physician, another physician, or other qualified healthcare professionals of the same specialty or subspecialty and belongs to the same practicing group within the past three years.
Codes from CPT 99211 – 99215 should be selected based on the current CPT Medical Decision Making table. Alternately, time alone may be used to determine the appropriate level of service. Total time for reporting these services includes face-to-face and non-face-to-face time personally spent by the Doctor or other health care professionals on the date of the encounter.
When using time for code selection, 20-29 minutes of the total time is spent on the date of the encounter.
The treating provider should document a medically appropriate history and physical examination. The right level of history and physical examination is no longer used when determining the level of service and is only used to make the level of E&M codes.
Providers report this 99213 CPT codefor established patients being seen in the Doctor’s office, a multispecialty group clinic, or other outpatient environments. Furthermore, CPT 99213 is the basic service, which entails Low-Level MDM with minor conditions. Using time for code selection of CPT 99213, 20-29 minutes of the total time should be spent on the date of the encounter.
The critical elements of service of E/M are:
- History
- Examination
- Medical decision-making
You do not need to take a complete history or physical exam to choose the level of Evaluation and management service level based on time unless it is medically necessary.
For example, if a patient returns to discuss the report findings of a test you ordered at a previous visit, you don’t need to repeat an entire history and exam at the current visit. Only document the total time of the visit and the time spent in counseling or coordination of care activities.
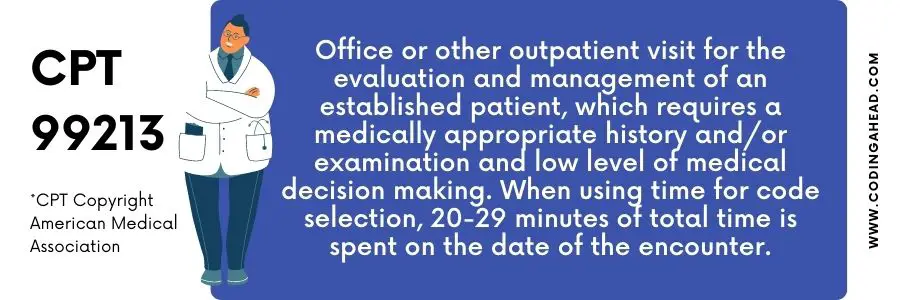
99213 CPT Code | Description
99213 CPT code -Office or other outpatient visits for an established patient (Evaluation & management) requires a medically appropriate history, examination, and Low-level (Medical decision making).
When using time for selecting the level of E&M code, then it should be between 20-29 minutes spent on the date of the encounter.
Selection Criteria of 99213 CPT code:
The proper level of E/M services for established patients is based on the criteria mentioned below.
History– Expanded problem-focused
Exam —-Expanded problem-focused
MDM — Low level
Two of the three critical above components must be fully documented to bill (other than 99211) when billing office or other outpatient services.
All the confronting and non–confronting time spent by the clinician on the day of the visit should be counted. Counseling should never be more than 50% of the total time.
Documentation Tips:
Only the medically necessary portion of the visit is allowed by Medicare. Therefore, even if a complete medical note is generated, only the essential services for the patient’s condition should be considered in determining the level of an E/M code at the time of the visit.
Medical necessity must be clearly stated and support the level of service reported.
99213 CPT Code | Reimbursement
The place-of-service (POS) codes for reporting these services are the same as those for a new patient: POS code 11 represents the clinician’s office environment, and POS code 22 means the outpatient setting.
When a separately identifiable E/M service is reported simultaneously as another procedure, modifier 25 should be used with the E/M service to indicate the service is distinct from the other service performed.
99213 CPT Code | Billing Guidelines
According to new billing guidelines, only two units per visit of CPT code 99213 are allowed to be billed. The second encounter on the same service date should be billed with 27 modifiers for commercial insurance.
The level of E&M service billed must be based on the treatment of a low level of complexity (having one self-limited or minor problem and straightforward MDM) performed concerning the medical care required by the reported symptoms and resulting in the patient’s diagnosis.
Cost and Relative value units of the facility services:
The Cost and total RVUs of CPT 99213 are $67.48 and 1.95000
respectively for both National and Global Facility Services.
Cost and Relative value units of the Non-facility services:
The Cost and total RVUs of Cpt 99213 are $92.05 and 2.66000
respectively for both National and Global Non-Facility Services.
Facility codes reflect the volume and ferocity of resources used by the facility to provide care.
Modifier 25 with Example
When another minor or major procedure is performed, a Separate identifiable Evaluation and Management service is carried out on the Same Day by the Same Physician or Other Qualified Health Care Professional.
Use modifier 25 on an E/M service performed during the same session as a preventive care visit when significant, separately identifiable E/M service is rendered in addition to the preventive care.
Use modifier 25 when the Evaluation and management service is Distinct, significantly identifiable, and separately documented as another service different from the E&M service.
Example:
An established patient presented to his family physician’s office with a 2.0 cm laceration of his right index finger. After the physician sutured the finger, the patient asked the physician to evaluate the swelling of his left leg and ankle. An expanded, problem-focused history and perform a physical examination with low complexity medical decision making. In this case, append modifier 25 with 99213.
Modifier 24 with Example
During a global fee period (postoperative) of an effective procedure, Unrelated Evaluation and Management service is carried out on the Same Day by the Same Physician or Other Qualified Health Care Professional.
Modifier 24 is appended with the E&M code when a patient is in the global fee period of a major or minor procedure performed within the global fee period. Still, They returned for a different condition or procedure with another Diagnosis code.
Example:
An office surgeon performed a total hip replacement on January 25. The procedure is significant and has 90 days global fee period, so all related postoperative treatment or follow-up is included in the payment for the hernia. But, on March 5, the patient returned to have a breast lump evaluated. In this case, append modifier 24 with 99213 CPT code E&M code if MDM is of low complexity.
Modifier 95 and GT
Both modifiers have almost the exact description and use. These are Synchronous Telemedicine Services provided through a Real-Time Interactive video or audio Telephonic, or telecommunication approach. Only the difference is Modifier 95 is used for Commercial insurance, and GT is used for Medicare.
Telemedicine service is a real-time interaction of a physician with the patient located far away from the physician’s office. Therefore, the information exchanged between the patient and physician or other qualified health care professionals during the telephonic communication service must be sufficient to meet the key components and requirements of the service when provided via direct face-to-face interaction.
So modifier 95 or GT should be appended to E&M service rendered via a telecommunication system.
Modifier 57 with Example
Modifier 57- “Decision for surgery.” An E&M service resulted in the decision to perform the significant/major surgery identified using a 57-modifier to the appropriate level of E/M service.
Use Modifier 57 to indicate an Evaluation and Management (E/M) service when the initial decision to perform surgery is the day before major surgery (90 days global) or the day of major surgery.
Example:
A 75-year-old established patient came to the Doctor’s office for a limited Range of motion in the hip joint and mild superficial tenderness and swelling on the lateral aspect of the hip; the Doctor performed an MRI and Bone density test that revealed a hairline fracture of the neck of the femur.
As a result, the Doctor decided to do the hip joint’s Hemiarthroplasty/partial hip replacement. So, in this case, append modifier 57 (decision for surgery) with 99213 CPT codeon the day because Partial hip replacement is a significant procedure and has a 90-day global period.
Billing Examples
The following are examples of when 99213 CPT code may be used.
Example 1 – Office visit for an established patient with new lesions of lichen planus in spite of topical therapies. (Dermatology)
Example 2 – Office visit for the quarterly follow-up of a 45-year-old lame with stable chronic asthma requiring regular drug therapy. (Allergy & Immunology)
Example 3 – Office visit for a 13-year-old, established patient, with comedopapular acne of the face that has shown poor response to topical medication, Discussion of use of systemic medication. (Dermatology)
Example 4 – Office visit for a 62-year-old female, established patient, for follow-up for stable cirrhosis of the liver. (internal Medicine/Family Medicine)
Example 5 – Office visit for a 3-year-old, established patient, with atopic dermatitis and food hypersensitivity for quarterly follow-up evaluation. The patient is on topical lotions and steroid creams as well as oral antihistamines. (Allergy & Immunology)
Example 6 – Office visit for an 80-year-old female, established patient, to evaluate medical management of osteoarthritis of the temporomandibular joint. (Rheumatology)
Example 7 – Office visit for a 70-year-old female, established patient, one year post excision of basal cell carcinoma of nose with nasolabial flap. Now presents with new suspicious recurrent lesion and suspicious lesion of the back. (Plastic Surgery)
Example 8 – Office visit for a 68-year-old female, established patient, with polymyalgia rheumatic, maintained on chronic low-does corticosteroid, with no new complaints.(Rheumatology)
Example 9 – Office visit for a 3-year-old female, established patient, for earache and dyshidrosis of feet. (Pediatrics/Family Medicine)
Example 10 – Office visit for an established patient for 18-months post-operative follow-up of TMG repair. (Oral & Maxillofacial Surgery)
Example 11 – Office visit for a 45-year-old male, established patient, being re-evaluated for recurrent acute prostatitis. (Urology)
Example 12 – Office visit for a 43-year-old male, established patient, with known reflex sympathetic dystrophy. (Anesthesiology)
Example 13 – Office visit for an established patient with an evenly pigmented superficial nodule of leg that is symptomatic. (Dermatology)
Example 14 – Office visit for an established patient with psoriasis involvement of the elbows, pitting of the nails, and itchy scalp. (Dermatology)
Example 15 – Office visit for a 27-year-old male, established patient, with deep follicular and perifollicular inflammation unable to tolerate systemic antibiotics due to GI upset, requires change of systemic medication. (Dermatology)
Example 16 – Office visit for a 16-year-old male, established patient, who is on medication for exercise-induced bronchospasm. (Allergy & Immunology)
Example 17 – Office visit for a 60-year-old, established patient, with chronic essential hypertension on multiple drug regimen, for blood pressure check. (Family Medicine)
Example 18 – Office visit for a 20-year-old male, established patient, for removal of sutures in hand. (Family Medicine)
Example 19 – Office visit for a 58-year-old female, established patient, with unilateral painful bunion. (Orthopaedic Surgery)
Example 20 – Office visit for a 45-year-old female, established patient, with known osteoarthritis and painful swollen knees. (Rheumatology)
Example 21 – Office visit for a 25-year-old female, established patient, complaining of bleeding and heavy menses. (Obstetrics & Gynecology)
Example 22 – Office visit for a 55-year-old male, established patient, with hypertension managed by a beta blocker/thiazide regime; now experiencing mild fatigue. (Nephrology)
Example 23 – Office visit for a 65-year-old female, established patient, with primary glaucoma for interval determination of intraocular pressure and possible adjustment of medication. (Ophthalmology)
Example 24 – Office visit for a 56-year-old man, established patient, with stable exertional angina who complains of new onset of calf pain while walking. (Cardiology)
Example 25 – Office visit for a 63-year-old female, established patient, with rheumatoid arthritis on auranofin and ibuprofen, seen for routine follow-up visit. (Rheumatology)
Example 26 – Office visit for an established patient with Graves’s disease, three months post I-131 therapy, who presents with lassitude and malaise.(Endocrinology)
Example 27 – Office visit for the quarterly follow-up of a 63-year-old male, established patient, with chronic myofascial pain syndrome, effectively managed by doxepin, who presents with new onset urinary hesitancy. (Pain Medicine)
Example 28 – Office visit for the biannual follow-up of an established patient with migraine variant having infrequent, intermittent, moderate to severe headache with nausea and vomiting, which are sometimes effectively managed by ergotamine tartrate and an antiemetic, but occasionally requiring visits to an emergency department. (Pain Medicine)
Example 29 – Office visit for an established patient after discharge from a pain rehabilitation program to review and adjust medication dosage. (Pain Medicine)
Example 30 – Office visit with 55-year-old male, established patient, for management of hypertention, mild fatigue, on beta blocker/thiazide regimen. (Family Medicine/Internal Medicine)
Example 31 – Outpatient visit with 37-year-old male, established patient, who is three years post total colectomy for chronic ulcerative colitis, presents for increased irritation at his stoma. (General Surgery)
Example 32 – Office visit for a 70-year-old diabetic hypertensive established patient with recent change in insulin requirement. (Internal Medicine/Nephrology)
Example 33 – Office visit with 80-year-old female, established patient, for follow-up osteoporosis, status-post compression fractures. (Rheumatology)
Example 34 – Office visit for an established patient with stable cirrhosis of the liver. (Gastroenterology)
Example 35 – Routine, follow-up office evaluation at a three-month interval for a 77-year-old female, established patient, with nodular small cleaved-cell lymphoma. (Hematology/Oncology)
Example 36 – Quarterly follow-up office visit for a 45-year-old male, established patient, with stable chronic asthma, on steroid and bronchodilator therapy. (Pulmonary Medicine)
Example 37 – Office visit for a 50-year-old female, established patient, with insulin-dependent diabetes mellitus and stable coronary artery disease, for monitoring. (Family Medicine/Internal Medicine)



