(2023) CPT Code 85025 | Description, Guidelines, Reimbursement, Modifiers & Examples
CPT code 85025 refers to the blood test as per the concerned physician’s order, and it includes the whole specimen of the blood of a specific patient. CPT 85025 involves a fully automated Blood Count (CBC) through an automated process using the related gadgets.
CPT Code 85025 | Description & Explanation
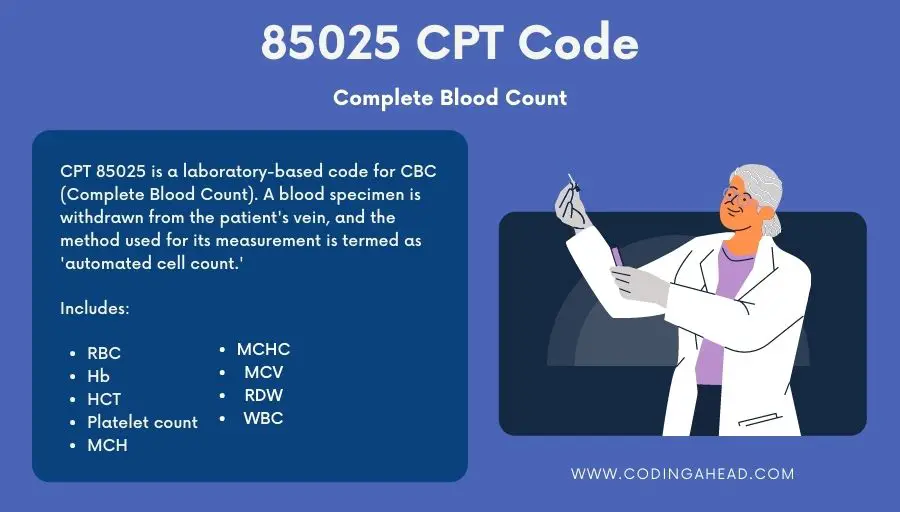
CPT 85025 is a laboratory-based code for CBC (Complete Blood Count). A blood specimen is withdrawn from the patient’s vein, and the method used for its measurement is termed an ‘automated cell count.’
Description: “Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC, and platelet count) and automated differential WBC count.”
The test includes the measurement of erythrocytes (RBCs or red blood cells), hemoglobin (Hb), Hematocrit (HCT or specific volume of packed RBCs or VPRC), thrombocyte count (platelet count), Corpuscular hemoglobin (MCH), Mean Corpuscular Hemoglobin Concentration (MCHC), Mean Corpuscular Volume (MCV), Red Cell Distribution Width (RDW) and fully automated differentiated leukocytes (WBC’s).
Remember that the differentiated leukocytes include granulocytes (neutrophils, eosinophils, basophils) and non-granulocytes (lymphocytes and monocytes).
It should be kept in mind that there is a slight difference between CPT Code 85025 and CPT 85027.
CPT 85025 includes an automated complete blood picture (CBC) with differential WBC count, whereas CPT 85027 includes an automated complete blood picture. The lab technician, the pathologist, and the physician, who order the test, must go as per the coding as the blood-related disorders are usually nonspecific. They should be precise in these issues.
A complete blood count (CBC) offers a detailed overview of different types of blood cells. A lab technician or a pathologist conducts this test by drawing blood from the patient’s vein with a syringe and storing it in a test tube with a proper amount of anticoagulant chemical, either citrate or EDTA.
Later, he sends it to the laboratory where a top-notch “automated analyzer” made from cutting-edge technology may be used to automatically count the number of cells.
The computing software related to this automated analyzer prints the results on paper through the attached printer so that the concerned physician can go through it without hassle.
Do consider that the collection procedure of the specimen, or the whole blood sample, is not part of a CPT 85025.
Billing Guidelines
Regarding billing, the covering (insurance) companies are pretty cautious about the slightest miscalculation or misinterpretation. In this regard, if the coding is incorrect, then the whole claim/bill can be wasted, resulting in insurance not being paid.
Here are some of the vital points that need proper consideration when you bill CPT code 85025 :
- CPT 85025 test means complete CBC, perfect blood count of WBC, RBS, hemoglobin, hematocrit, and platelets, and an automated WBC count differential. An average fee for this test is normally $10 to $20, though the fee may vary due to varying factors.
- Comprehensive Error Rate Testing (CERT) report has recently indicated errors in coding CPT code 85025 and mixing things with CPT 85027. Therefore, it is highly recommended that the concerned physician’s order must be followed. However, the pathologist may sometimes take an on-the-spot decision in case of the indication of some abnormal behaviour of some type of blood cells.
If the physician primarily uses CBC, why include the differential in the bill?
The coders must strictly follow the recommended guidelines and include only the correct codes to avoid future issues, as the cover-providing auditors would analyze their reports. Moreover, never refer to the physician’s initial order in the report so that your documentation shows no lapse.
And, for correct coding, you may consult National Correct Coding Initiative (NCCI) edits to receive your expected payments without any issues involved in this regard. Better to avoid the bundled testing type of billing when preparing a report for the test codes CPT 85004, CPT 85025, and CPT 85027.
Do not bill the following CPT codes along with CPT 85025 when finally billing; CPT 85004, CPT 85007, CPT 85008, CPT 85009, CPT 85013, CPT 85014, CPT 85018, CPT 85027, CPT 85032, CPT 85041, CPT 85048, CPT 85049, CPT 88738, CPT G0306 or CPT G0307.
Following are the topmost diagnosis with ICD 10 codes that can be billed as primary diagnoses:
- ICD 10: D50.9 => Iron deficiency anemia, unspecified
- ICD 10: D64.9 => Anemia, unspecified
- ICD 10: E03.9 => Hypothyroidism, unspecified
- ICD 10: E11.65 => Type 2 diabetes mellitus with hyperglycemia
- ICD 10: E11.9 => Type 2 diabetes mellitus without complications
- ICD 10: E53.8 => Deficiency of other specified B group vitamins
- ICD 10: E55.9 => Vitamin D deficiency, unspecified
- ICD 10: E78.00 => Pure hypercholesterolemia, unspecified
- ICD 10: E78.2 => Mixed hyperlipidemia
- ICD 10: E78.5 => Hyperlipidemia, unspecified
- ICD 10: I10 => Essential (primary) hypertension
- ICD 10: I25.10 => Atherosclerotic heart disease of native coronary artery without angina pectoris
- ICD 10: N18.30 => Chronic Kidney Disease stage 3 unspecified
- ICD 10: N39.0 => Urinary tract infection, site not specified
- ICD 10: R53.83 => Other fatigue
- ICD 10: R73.01 => Impaired fasting glucose
- ICD 10: R73.03 => Prediabetes
- ICD 10: R73.09 => Other abnormal glucose
- ICD 10: R73.9 => Hyperglycemia, unspecified
- ICD 10: Z79.899 => (Other long term (current) drug therapy)

Does CPT code 85025 need modifiers?
CPT 85025 is a high-quality Clinical Laboratory Improvement Amendment (CLIA) waived lab test. The Modifier QW indicates the diagnostic lab service of CLIA waived test, and the provider must have the legal Certificate of Waiver to perform this test.
While performing the QW modifier test, do ensure to use the CPT 87880 CLIA waived kit and see if the kit manufacturer is listed there and, later on, add the precise code in the report.
Now, let’s talk about the most the reimbursement fees for CPT 85025.
Reimbursement
Reimbursement of the funds depends largely on precise coding on your part and also considering whether the CPT 85025 test is with or without differential.
Maximum reimbursement for CBC with automated differential for CPT code 85025 is $10.69.
- CPT code 85025: $7.77
- QW CPT code 85025: $7.77
- CPT code 85027: $6.47
Note: The test price may change in specific circumstances.
When going through the blood test, the physician must also consider the required indications for the test; some of which are as follows:
The CBC indications include malfunctions and disorders relating to the red blood cells, platelets, and white blood cells of the specific patient whose blood has been withdrawn.
Note:
- New-fangled CPT G0306 is billed at a similar amount as CPT 85025.
- New-fangled CPT G0307 is billed at a similar amount as CPT 85027.
Well, the time has come now when we may talk about the CBC recommendation requirements in general.
CBC is recommended when:
- There is an evaluation of the dysfunction of bone marrow either due to pregnancy, immunity issues, or exposure to toxic substances in any condition whatsoever.
- They treat illness, weight loss, pallor, fatigue, continuous bleeding, blood loss in large quantities, abnormal menstrual bleeding, hematuria, malabsorption, malnutrition, etc.
- Having heart headache, murmur, wheezing, cyanosis, chills, fever, ruddy skin, cough, orthopnea, vague cognitive changes, excessive sweating, etc.
- You are dealing with varying ailments like mucopolysaccharidoses, drug addicts, leukocytosis (G-CSF or CM-CSF), etc.
- There is testing asymptomatic patients resulting in hematological abnormality.

Billing Examples
Example 1: A patient comes for a CBC only per the physician’s advice or order. The laboratory runs CBC for CPT code 85025 and automated differential and bills for both.
What would the covering company’s auditors do?
The audit-related personnel is sure to follow the physician’s order. They will presume the lab technician’s fault in taking the automated differential test and allow the cover company to be billed according to the Comprehensive Error Rate Testing (CERT) rules. This would, of course, lead the coder or the provider to dismay over the issue.
Example 2: A diabetic patient with kidney issues comes with the physician’s order of a CPT 85025 and CPT 85027 and a complete CBC.
What is the lab technician’s duty?
The lab technician must follow the doctor’s order, do what is told, and not stray or trespass to the specified limits. He may, in this case, consult the concerned pathologist, too.
Performing extra tests will not benefit the provider in any way, and the lab technician or the pathologist has to ensure that the required tests are performed as per the requirements of the physician who originally ordered them.
Example 3: A patient with some unknown ailment comes around, and the physician has to order a general CPT test.
What type of tests are required initially?
Suppose the signs of ailment or some malfunctioning organs are not properly visible in some specific patient, although he or she has an ailment. In that case, the physician has to order a single CBC test, which may be appropriate initially.
Example 4: Repeated testing may not be indicated unless abnormal results are found, or there is a change in the physical condition of the blood. If repeated testing is performed, as related to the general behavior of the human body and to order for more tests after analyzing and evaluating the initial test.
In this case, a descriptive diagnosis code like anemia and the CPT 85025 should be prescribed, and the same should be reported later to the doctor who ordered it.
What if there are abnormal results when testing a specific patient’s blood?
In such a scenario, CBC may be the solution in the beginning. If there are indications of abnormal results, repeated tests may be performed as per the requirement to avoid the risks of hematologic abnormality.
Inappropriate use of CPT 85025
Below are some examples of CPT 85025 usage by laboratory and provider office, and we will learn how this CPT is commonly misused and abused in outpatient healthcare claims.
Example of misuse: A minor mistake while choosing this CPT to represent the service will lead to the misuse of the CPT, i.e., A provider ordered a complete CBC for a patient with acute febrile illness to see the root cause of the patient’s illness, and it is represented in the claim.
CPT 85025 includes a complete blood count in addition to a differential count of WBC. As the physician did not order the differential count, it will lead to the misuse of the CPT and an overpayment. As a result, anytime insurance calls an audit, it can lead to a penalty because the provider will be unable to provide the documentation supporting this level of service.
Example of Abuse: Per the CMS guidelines, a Service is considered abuse when it is not proved with the medical necessity concerning the local coverage determination.
We have to educate the physicians regarding selecting this pathology service as if the differential count of the white blood cells is required for medical decision-making.
The most common example is acute laryngitis vs. follicular tonsillitis. A physician may order a CBC test for acute laryngitis represented by 85027 for medical decision-making as it does not include the White blood cells differential count.
But if a coder perceives it as CBC with a white blood differential count of CPT code 85025 and uses acute laryngitis, it will prove the medical necessity. Still, it will lead to overpayment and abuse of CPT 85025.
The tests of CPT code 85025, CPT 85027, CPT 85007, etc., may also be considered for this purpose. Majorly the physician has the deciding power, and the lab technician and the pathologist have to follow suit. The ordering physician may also be consulted in such a situation to avoid any mishap in this connection.
In line with the rules mentioned above and instances, a provider or the coder may expect to get the company’s desired reimbursement if the same followed precise rules and regulations when preparing the report exhibiting correct ICD (international classification of diseases) and CPT (Current Procedural Terminology) codes.