(2022) How To Code Elevated Liver Enzymes ICD 10 – List With Codes & Guidelines
Elevated liver enzymes ICD 10 coding is made easier with our billing guidelines. This article includes all medical codes you will need to report elevated liver enzymes and related specific ICD 10 codes such as elevated liver enzymes in pregnancy. Read on for a summary of the necessary codes followed by a description.
What Are Elevated Liver Enzymes?
Elevated liver enzymes ICD 10 are generally a sign of inflammation or harm to liver cells. An increase in liver enzymes may be shown on blood tests when the liver is inflamed or damaged.
The term “elevated liver enzymes” refers to elevated amounts of liver enzymes in the blood. In rare cases, high liver enzyme levels may indicate the presence of a more severe medical condition such as hepatitis or liver disease.
Drugs may also induce elevated liver enzymes. Proteins known as liver enzymes speed up the chemical reactions in your body.
Chemical processes include the production of bile and substances that aid in blood coagulation, the breakdown of food and contaminants, and disease prevention. Liver enzymes may arise for various causes, including liver disease and medication.
There is also the possibility of transient increases in liver enzymes. If your blood test shows abnormal levels of liver enzymes, see your doctor. They’re going to attempt to figure out what’s causing the issue.
Cholestatic liver disease may be classified as extrahepatic or intrahepatic based on the findings of the tests. Extrahepatic cholestasis may be caused by obstruction of the bile ducts owing to stones or cancer.
Intrahepatic cholestasis may be caused by various things, including viral and alcoholic hepatitis, nonalcoholic steatohepatitis, alkylated steroids, herbal supplements, and infiltrative diseases such as amyloid sarcoid lymphoma, tuberculosis, and primary biliary cholangitis.
A variety of tissues, including bones, kidneys, intestines, and the placenta, contain the enzyme alkaline phosphatase. It may be elevated during pregnancy, adolescence, and after fatty meals because of intestinal release.
If isolated alkaline phosphatase elevations are discovered, GGT or 5-nucleotidase, more specific for liver illness, should be evaluated. If alkaline phosphatase levels are within normal limits but not originating from the liver, this enzyme should be investigated further.
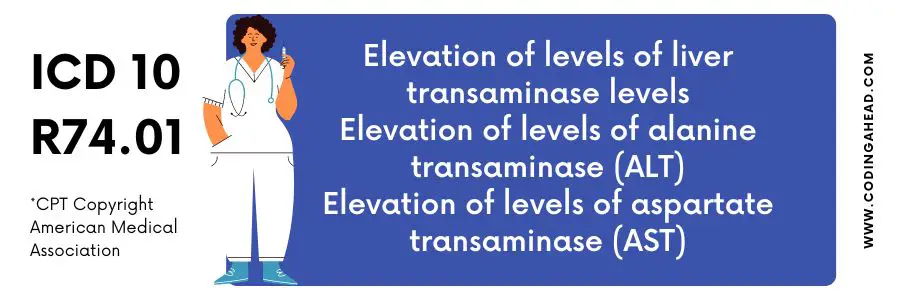
Elevated Liver Enzymes ICD 10
The ICD 10 code for Elevated Liver Enzymes is R74.01.
Liver enzymes may be discovered to be high during regular blood testing. Liver enzyme levels are often only modestly elevated and for a brief time. In most cases, elevated liver enzymes are not indicative of a long-term or serious liver problem.
In clinical practice, high levels of hepatic enzymes are often seen. The most common reasons for a rise in liver enzymes include alcoholism, pharmacological overdose, and a fatty liver.
The pattern of enzyme increase may distinguish hepatocellular damage and cholestatic diseases.
Hepatocellular injury increases alanine and aspartate aminotransferases (ALT and AST). In addition, increased levels of alkaline phosphatase, ferritin, bilirubin, and gamma-glutamyl transferase (GGT) have been seen in patients with cholestatic diseases.
If a person’s liver enzyme levels are high, it is conceivable that their liver is failing. A blood test may be used to identify enzymes produced by damaged or inflamed liver cells. If a patient exhibits indicators of liver illness, physicians will perform a liver enzyme test on the patient.
When increased liver enzymes are detected in blood testing, a doctor must investigate the source of the elevated enzyme levels.
People’s lifestyle and dietary habits may be inquired about in addition to another testing. Fatty liver disease is the most prevalent reason for increased levels of liver enzymes.
This condition was present in 25–51 percent of persons who had increased liver enzyme levels. Fatty liver disease is caused by fat accumulation in the liver tissue. If alcohol is involved, the condition is an alcoholic fatty liver disease.
Nonalcoholic fatty liver disease (NAFLD) is a kind of fatty liver disease caused by anything other than alcohol use (NAFLD). People with metabolic syndrome are more prone to acquire NAFLD than the general population.
A typical indication of fatty liver disease is fatigue, which may manifest as discomfort on the right side of the abdomen. However, these symptoms are often overlooked by patients.
According to the American Liver Foundation, patients with increased liver enzymes, a history of alcohol misuse, or metabolic syndrome may be diagnosed with fatty liver disease.
What Are Elevated Liver Enzymes In Pregnancy?
Pregnant women’s liver enzymes change throughout time, but long-term studies on insulin resistance and the risk of gestational diabetes (GDM) are lacking.
As a result, gynecologists and hepatologists face an uphill battle when trying to learn more about the elevated liver disease during pregnancy. Nevertheless, it is estimated that around 3% of pregnant women may have some kind of liver disease.
This list contains a few dangerous conditions for pregnant women and their babies. In addition, there are three types of liver problems that must be recognized during pregnancy.
Pregnancy-related liver illness might manifest itself throughout your pregnancy and can be fatal. In addition to being aware of the possibility of non-pregnancy-related liver illness, such as viral or drug-induced hepatitis, you should be aware that it may strike at any time.
According to research, women who have previously been diagnosed with liver illness are more likely to become pregnant. Based on a single liver function test, it is difficult to make a definitive diagnosis of liver disease.
In medicine, the phrase “liver function tests” refers to tests used to evaluate different aspects of liver health and function.
Health care providers may have a tough time dealing with pregnancy-related liver disease.
Of course, you are pregnant has been associated with a range of liver disorders, but it is not the only factor to consider. In addition to hemolysis and hyperemesis gravidarum, there are other pregnancy-specific liver problems to be aware of.
These include acute fatty liver of pregnancy (AFLP), intrahepatic cholestasis (ICP), and intrahepatic cholestasis (IHC). Furthermore, HELLP syndrome is a medical condition that requires treatment.
To reduce the risk of pregnancy-induced liver illness such as acute viral hepatitis for pregnant women with chronic liver disease such as cirrhosis and portal hypertension, liver transplant recipients, and those who have had a liver transplant (acute viral liver disease).
Diagnosis of liver anomalies in pregnant women requires the same level of diagnostic examination as for non-pregnant patients, but with the additional concerns of gestational age and the expected physiologic changes during pregnancy.
The ACG’s recommendations govern imaging and endoscopy in pregnant women: Having high liver biochemistry and function tests in pregnant women might be a problem for the consulting physician.
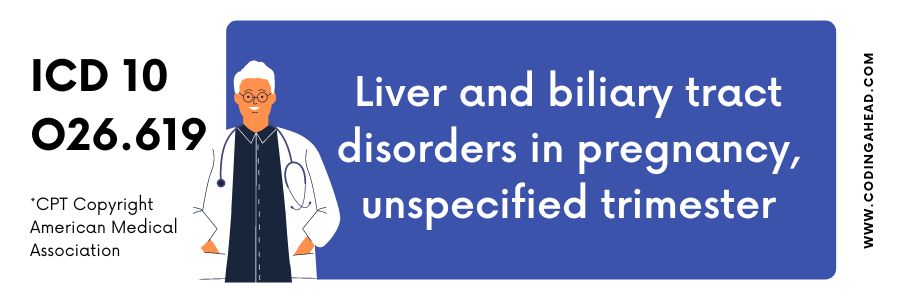
Elevated Liver Enzymes In Pregnancy ICD 10
The ICD 10 code for Elevated Liver Enzymes in Pregnancy is O26.619.
Changes in the liver’s biochemical profile are frequent during pregnancy. Even though it is rare, severe liver disease may develop and must be recognized early to prevent harm to the mother and the infant.
Pre-existing liver disease may significantly influence a pregnant woman’s health, as are the most frequent liver illnesses associated with pregnancy. Serum albumin concentration decreases during normal pregnancy, linked with increased total plasma volume.
After the baby is delivered, this may continue for months. In addition, two- to fourfold increases in serum alkaline phosphatase (ALP) levels are seen. Placental production has a role here.
As long as there are no anomalies in the levels of the enzymes ALT, AST, bilirubin, or GGT, the patient should be considered healthy for further testing. For pregnant women, early detection of conditions connected to the liver and the hepatic system may significantly minimize the risk of complications for both mother and child.
There is no evidence to suggest that transabdominal hepatic ultrasonography has any negative effects on the fetus and is thus the primary choice for pregnant women who have abnormally high liver biochemistry and function tests.
We also use Doppler ultrasonography to rule out hepatic or portal vein thrombosis in patients with suspected vascular disease (e.g., right upper quadrant pain, ascites).
Noncontrast magnetic resonance imaging (e.g., magnetic resonance cholangiopancreatography) is preferable over computed tomography (CT) in patients with suspected biliary obstruction or cholangiopathy, but nondiagnostic ultrasound or certain individuals with abnormal ultrasound (e.g., liver mass).
We avoid using gadolinium-containing contrast agents because this metal might injure an unborn child if it enters the placenta. In addition, maternal and fetal death rates have increased due to several uncommon diseases.
The liver ailment is promptly cured thanks to the timely supply of the medication. Penicillamine, trientine, prednisone, and azathioprine are safe for pregnant women.
Liver functions include the biotransformation and elimination of insoluble substances (such as drugs, toxins, and the colourless yellow bilirubin), the production of plasma proteins (such as albumin, coagulation factors, alpha and beta-globulins, and transferrin), the metabolism of cholesterol and the metabolism of amino acids, carbs, and lipids, among other things.



