A Comprehensive Guide to Zoonotic Bacterial Diseases
The sections below represent summaries of Zoonotic Bacterial Diseases. First we’ll cover Plague, followed by Tularemia, Anthrax, Brucellosis, Glanders and melioidosis, Rat-bite fevers, Erysipeloid, Leptospirosis icterohemorrhagica, and Other zoonotic bacterial diseases.
1. Plague
Plague is a severe bacterial infection caused by the bacterium Yersinia pestis and is typically acquired through the bite of infected fleas, contact with contaminated fluid or tissue, or inhaling airborne infectious droplets.
There are three primary forms of plague:
- Bubonic, which involves the lymph nodes;
- Septicemic, in which the infection enters the bloodstream and
- Pneumonic, which involves the lungs.
Plague can also involve the skin and sometimes the central nervous system.
1.1 Symptoms
A patient with plague experiences flu-like symptoms with;
- fever;
- chills;
- headache; and
- muscle pain.
The patient may become extremely weak, shocked, and even die in severe cases.
1.2 Diagnosis
Laboratory tests of blood, sputum, and pus from an infected lymph node (bubo) or lymph node tissue can detect the Yersinia pestis bacterium; specific antibody tests for Y. pestis may also be performed.
1.3 Treatment
Treatment includes rehydration with oral or intravenous fluids and antibiotics, and in case of any complication, respiratory support and hospitalization may be required. Vaccination is available for healthcare workers and people who live or work in endemic areas but is not recommended for the general population.
2. Tularemia
Tularemia, also known as rabbit fever or deerfly fever, is a rare bacterial infection caused by Francisella tularensis;
- transmitted from infected rodents and other wild and domestic animals through infected ticks or flying insect bites;
- by direct entry of the bacteria through cuts or sores;
- by touching the eyes or mouth with unwashed hands after handling infected dead animals; or from
- the bacteria entering the bloodstream from other infected sites.
2.1 Symptoms
Specific symptoms of tularemia depend on the type, but in general, a patient with tularemia can experience;
- the sudden onset of fever and chills;
- headache;
- backache;
- muscle and joint pains;
- sweats;
- red lesions that turn into open sores;
- difficulty breathing;
- extreme exhaustion;
- sore throat;
- loss of appetite;
- vomiting; and
- weight loss.
Various forms of tularemia are characterized by;
- lymph node involvement with skin ulcers (ulceroglandular) or without (glandular);
- eye involvement with swollen lymph nodes (oculoglandular);
- lung involvement (pneumonic);
- gastrointestinal involvement; and
- involvement of bones (osteomyelitis), heart (pericarditis), and central nervous system (meningitis).
2.2 Diagnosis
A provider diagnoses a patient based on the patient’s history, symptoms, physical examination, and signs.
Laboratory tests include blood culture, serologic tests, polymerase chain reaction (PCR) for antibody identification, and microscopic analysis of specimens taken from lymph nodes or lesion biopsies. A chest X–ray may be performed to assess pulmonary involvement.
2.3 Treatment
Treatment includes antibiotics such as doxycycline, ciprofloxacin, streptomycin, and tetracycline.
3. Anthrax
Anthrax, a rare but severe infection that affects the skin, respiratory, and gastrointestinal systems, is caused by the bacterium Bacillus anthracis, which typically spreads in the human body as spores inhaled.
At the same time, breathing is ingested with contaminated water and food or enters through a cut in the skin.
3.1 Symptoms
A patient with anthrax can experience;
- fever and chills;
- nausea and vomiting;
- stomach pain;
- headache;
- profuse sweating;
- lethargy;
- confusion;
- cough;
- shortness of breath;
- chest discomfort;
- body ache; and
- in severe and untreated cases, the patient may even die.
3.2 Diagnosis
The provider diagnoses the patient based on history and physical examination. Laboratory tests of the patient’s blood, spinal fluid, respiratory secretions, or skin specimens can detect the toxins of the B. anthracis bacterium.
The provider may perform a chest X–ray or CT scan in case of inhalation of anthrax.
3.3 Treatment
Treatment includes using antibiotics and antitoxins to kill the toxins the bacterium produces in the patient’s body. Providers may vaccinate at–risk individuals with the Anthrax Vaccine Adsorbed (AVA) to protect against cutaneous and inhalation anthrax.
4. Brucellosis
Brucellosis is an infectious zoonotic disease caused by bacteria of the genus Brucella, typically ingested with undercooked meat or unpasteurized dairy products, inhaled while breathing or entered through skin wounds. Brucellosis may also be called Malta, Mediterranean, or undulant.
There are primarily four species of Brucella that cause disease in humans, listed by degree of pathogenicity (ability to cause disease) and severity of infection: B. melitensis from sheep, B. suis from pigs, B. abortus from cattle, and B. canis from dogs.
4.1 Symptoms
A patient with brucellosis can experience;
fever, headache, muscle and joint pain, sweats, fatigue, malaise or uneasiness, and anorexia (loss of appetite). Neurologic symptoms, such as mental status changes, stiff neck, seizures, and even coma, may also occur, as may psychiatric symptoms, such as depression. Intestinal, urinary, and cardiac symptoms may be present as well.
4.2 Diagnosis
The provider diagnoses the patient based on symptoms, history, and physical examination. Laboratory tests of the patient’s blood, urine, and spinal fluid can detect antibodies to the Brucella bacterium. The provider may perform a bone marrow culture.
4.3 Treatment
Treatment includes the use of antibiotics. Providers may educate the patient on disease prevention by avoiding the consumption of undercooked meat or unpasteurized milk and milk products and by wearing protective gloves, masks, glasses, or aprons when handling animals.
5. Glanders and melioidosis
Bacteria of the genus Burkholderia, which typically enter the human body through cuts in the skin or mucosa of eyes and nose or are inhaled while breathing, cause glanders and melioidosis, an infectious disease transmitted to humans through contact with infected animals; B. mallei cause glanders and B. pseudomallei causes melioidosis.
5.1 Symptoms
Symptoms are nonspecific and make diagnosis difficult.
A patient with glanders or melioidosis can experience;
- fever;
- night sweats;
- muscle pain;
- rigors (shaking chills);
- anorexia (loss of appetite);
- headache;
- chest pain;
- cough;
- sensitivity to bright lights;
- excessive tearing, and
- diarrhea.
Patients with melioidosis may exhibit hives and reddish welts on the skin.
If the infection enters the bloodstream, the patient may experience;
- flushing (extreme redness of the skin) and purulent (pus–filled) lesions on the skin;
- enlarged and/or inflamed lymph nodes; and
- cellulitis (inflamed, open sores that extend into the subcutaneous tissue and sometimes down to muscle).
5.2 Diagnosis
Laboratory tests of the patient’s blood, urine, sputum, and skin specimens can detect the bacterium.
5.3 Treatment
Treatment includes antibiotics such as amoxicillin, doxycycline, or trimethoprim–sulfamethoxazole (TMP–SMX).
When handling animals, providers may educate patients on disease prevention by wearing protective gloves, masks, glasses, or aprons.
6. Rat-bite fevers
Rat–bite fever (RBF) is an infectious disease transmitted by infected rodents through skin scratches and bites or ingested with contaminated food or water.
Two bacteria can cause RBF:
- Streptobacillus moniliformis causes streptobacillary RBF
- Spirillum minus causes spirillary RBF or sodoku.
6.1 Symptoms
A patient with rat–bite fever can experience various symptoms depending on the type of RBF.
Patients with streptobacillary RBF, which is more common in North America, may have;
- fever;
- vomiting;
- headache;
- muscle and joint pain; and
- skin rash.
Patients with spirillary RBF, more common in Asia, can experience;
- remitting and relapsing fever;
- ulcer formation and swelling around the bite wound;
- lymph node swelling; and
- skin rash after partial wound healing.
The patient may develop an earnest heart, brain, or lung infection in severe cases.
6.2 Diagnosis
Providers diagnose the condition based on the patient’s exposure history and physical examination. Laboratory tests of the patient’s blood, synovial, or other body fluids can detect the bacterium.
6.3 Treatment
Treatment includes the use of antibiotics, most commonly penicillin. Providers may educate patients to avoid consumption of possibly contaminated food or water and not to drink raw (unpasteurized) milk.
7. Erysipeloid
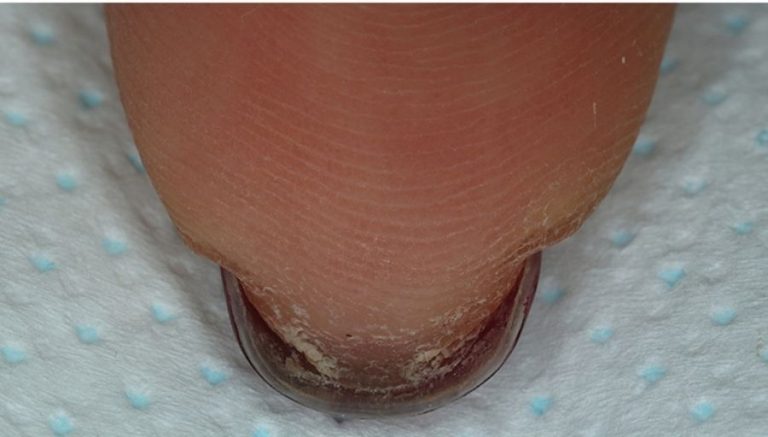
The bacterium Erysipelothrix rhusiopathiae, typically spread from animals such as fish, birds, and shellfish to humans, causes erysipeloid, an inflammation primarily affecting the patient’s skin.
The disease commonly affects farmers, butchers, cooks, and homemakers.
7.1 Symptoms
A patient with erysipeloid can experience;
- warmth;
- tenderness,;
- erythema or swelling;
- burning sensation;
- pain, and redness on the skin;
- in case of generalized infection, the patient may experience;
- fever;
- chills;
- weight los;
- joint pain;
- cough; and
- a headache.
7.2 Diagnosis
The culture of the patient’s skin specimen can detect the Erysipelothrix rhusiopathiae bacterium; PCR amplification may be helpful in rapidly diagnosing systemic infection.
7.3 Treatment
Treatment includes the use of antibiotics, especially penicillin.
8. Leptospirosis icterohemorrhagica
The bacterium Leptospira, typically ingested with water contaminated by animal urine or spread through contact with the infected soil, causes leptospirosis icterohemorrhagica. This infectious zoonotic disease may also be called Weil syndrome and results in jaundice and bleeding lesions, primarily occurring in warm climates.
Leptospirosis icterohemorrhagica is also referred to as:
- Leptospiral or spirochetal jaundice (hemorrhagic)
- Weil’s disease
8.1 Symptoms
A patient with leptospirosis icterohemorrhagica can experience;
- fever and chills;
- jaundice (yellow discoloration of skin and whites of the eyes from excess bilirubin in the blood);
- hemorrhagic (bleeding) lesions;
- headache;
- nausea;
- vomiting;
- diarrhea;
- muscle pain;
- dry cough; and
- abdominal pain.
8.2 Diagnosis
Laboratory tests of the patient’s blood can detect antibodies to the Leptospira bacterium.
8.3 Treatment
Treatment includes doxycycline or penicillin; intravenous antibiotics may be given in severe cases.
Providers may educate the patient on preventing the disease by avoiding areas with stagnant water, not swimming in water contaminated by animal urine, and wearing proper clothing when in contact with potentially infected soil or water.
9. Other zoonotic bacterial diseases
Certain bacteria, typically ingested with water contaminated by animal urine or spread through contact with the infected soil, cause zoonotic diseases, which are animal diseases that can be spread to humans under certain natural conditions.
9.1 Symptoms
A patient with zoonotic bacterial diseases can experience;
- fever and chills;
- headache;
- nausea;
- vomiting;
- diarrhea;
- muscle pain;
- dry cough; and
- pain in the abdomen.
9.2 Diagnosis
Laboratory tests of the patient’s blood can detect antibodies to the bacterium.
9.3 Treatment
Treatment includes doxycycline or penicillin; intravenous antibiotics may be given in severe cases.
Providers may educate the patient on preventing the disease by avoiding areas with stagnant water, not swimming in water contaminated by animal urine, and wearing proper clothing when in contact with potentially infected soil or water.